Understanding Perimenopause: Your Next Chapter
Reading time 8 min

Reading time 8 min

Have you been feeling different lately? Maybe your periods are changing (getting longer, shorter, or irregular), or you’re experiencing mood swings and fatigue without a tangible reason? Perhaps you’re waking up in the middle of the night, drenched in sweat, or finding it harder to fall asleep than before. These changes might seem puzzling, but they actually are your body’s way of signaling a new chapter called perimenopause.
What is perimenopause?
Perimenopause is the transition phase leading up to menopause, marked by hormonal changes that affect periods, mood, sleep, and body functions. It typically starts in a woman’s 40s and can last several years.
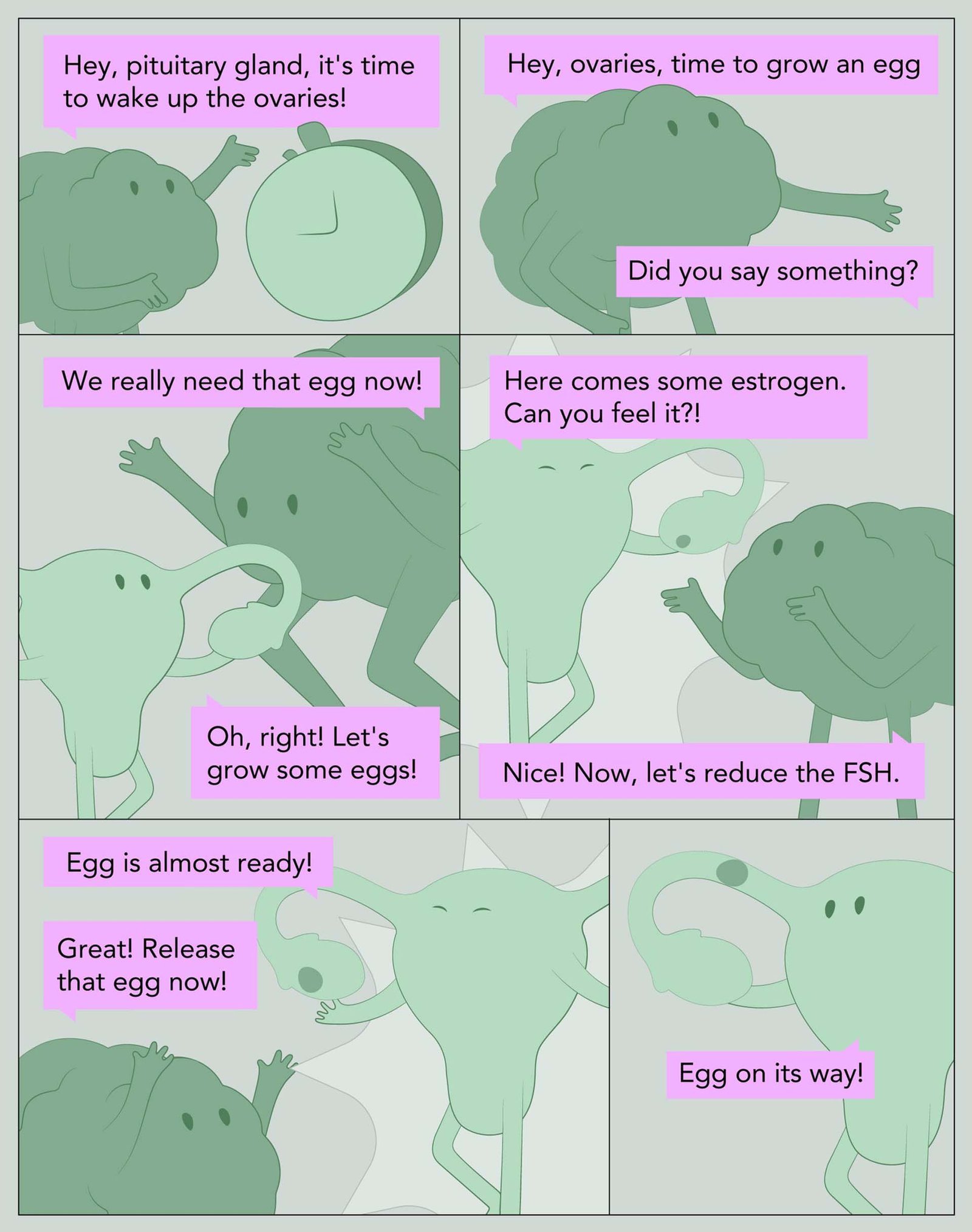
It all begins in the womb. Not yours, but your mother’s, where around 6 to 7 million eggs are formed in your developing ovaries. By the time you are born, this number drops to about 1 to 2 million. Each egg is held inside a follicle, which is like a tiny nest. Starting in puberty, your brain sends a signal (initiates a chat) to your ovaries using Follicle-Stimulating Hormone (FSH). FSH encourages a few follicles to grow and mature, each holding one egg.
As the follicles develop, they produce estrogen. Once an egg is fully mature, Luteinizing Hormone (LH) triggers ovulation – the release of the egg from its follicle, ready to begin its journey. After ovulation, the now-empty follicle starts producing progesterone to prepare your body for pregnancy. This communication between your brain and ovaries is called the Hypothalamic-Pituitary-Ovarian (HPO) axis.
Imagine a conversation between your brain and ovaries:
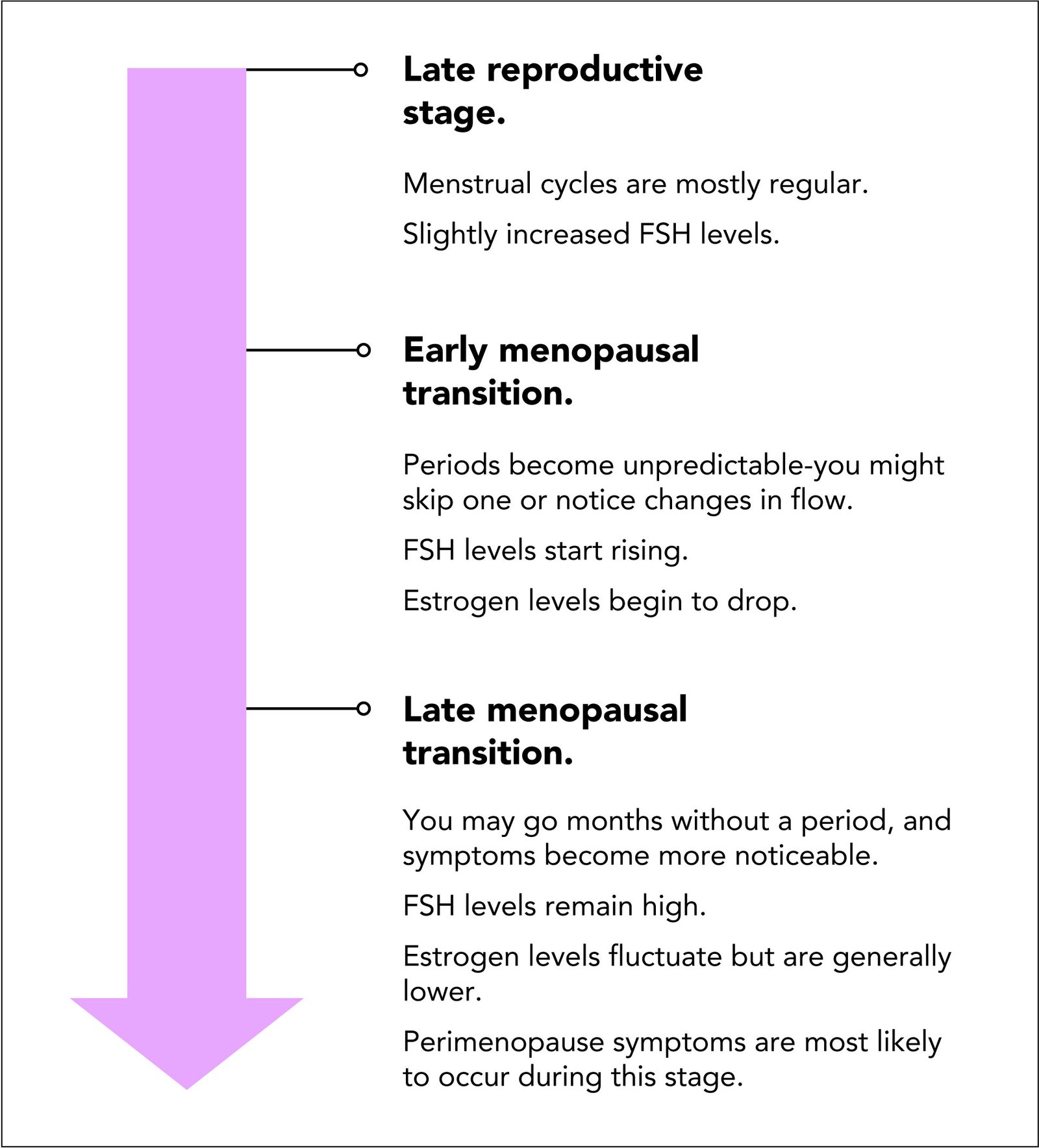
As you near menopause, the conversation between the brain and your ovaries begins to slow down. The slowing down marks the beginning of perimenopause. Perimenopause usually begins in your 40s, but it can start earlier for some women 1, 2, 3, 4, 5, 6, 7. It can last anywhere from 1 to 12 years5.
With fewer eggs remaining, the follicles become less responsive to FSH, and estrogen and progesterone production starts to decline2, 4. This creates a vicious cycle: fewer eggs lead to less hormone production, which leads to irregular cycles, and this cycle repeats until ovulation and hormone production stop completely9, 10, 11. These changes affect not just your periods but many parts of your body, causing new and sometimes surprising symptoms.
Perimenopause can be divided into three stages: late reproductive stage, early menopausal transition, and late menopausal transition12, 13.
Note: Other conditions can cause menstrual irregularities, such as thyroid disease, pregnancy, or hormonal contraceptive use. Always consult a healthcare provider to rule out other possibilities.
Perimenopause can manifest in various ways, from clear physical symptoms to more subtle changes that you might not immediately connect to hormonal shifts. Understanding the signs – both the obvious and the hidden – can help you recognize what’s happening and take proactive steps toward feeling your best.
You might notice one, many, or none of the signs of perimenopause, and those symptoms can come in different intensities. Sometimes, it’s hard even to connect them to perimenopause. Many women often feel isolated and think something is wrong with them when they start feeling “off” instead of appreciating it as their body goes through natural biological changes14.
Have you experienced any of the below?
Here’s a full list of symptoms that you, like many perimenopausal women, might experience.
Not all perimenopause symptoms are immediately noticeable, but they can still have a big impact on your health:
By taking these steps, you’re not just easing current symptoms – you’re investing in your long-term health. You’ll reduce the risk of serious conditions like heart disease, osteoporosis, and certain cancers. Plus, you’ll feel more empowered and in control of your life.
Perimenopause cannot be diagnosed with a simple blood test. I wish it were that easy! I do talk about hormones and tests on this website, but in this case, perimenopause is a collection of symptoms – unique, yet similar for every woman. Perimenopause isn’t just an ending, although there are moments when it feels like you can’t find yourself in the chaos.
Think of it as the start of a new journey. It’s your body’s way of saying, “It’s time to focus on you.” You might think that’s a luxury or not something you need. But trust me, it is! Embrace this phase as a chance to understand yourself better and prepare for the future. Remember, the actions you take today will shape your tomorrow – not just any tomorrow, but a vibrant, no-excuses tomorrow.
Dr. Jūra Lašas
1.
Willi, J. et al. The Swiss Perimenopause Study – Study Protocol of a Longitudinal Prospective Study in Perimenopausal Women. (2020) https://doi.org/10.1186/s40695-020-00052-1
2.
Brinton, R. et al. Perimenopause as a Neurological Transition State. (2015) https://doi.org/10.1038/nrendo.2015.82
3.
Frackiewicz, E. et al. Women’s Health Care During the Perimenopause. (1996) https://doi.org/10.1016/S1086-5802(16)31127-5
4.
Grub, J. et al. Steroid Hormone Secretion Over the Course of the Perimenopause: Findings From the Swiss Perimenopause Study. (2021) https://doi.org/10.3389/fgwh.2021.774308
5.
Randolph, J. et al. Change in Follicle-Stimulating Hormone and Estradiol Across the Menopausal Transition: Effect of Age at the Final Menstrual Period. (2011) https://doi.org/10.1210/jc.2010-1746
6.
McNamara, M. et al. Perimenopause. (2015) https://doi.org/10.7326/AITC201502030
7.
Santoro, N. Perimenopause: From Research to Practice. (2016) https://doi.org/10.1089/jwh.2015.5556
8.
Visser, J.et al. Anti-Müllerian Hormone and Folliculogenesis. (2005) https://doi.org/10.1016/j.mce.2004.09.008
9.
Sherman, B. et al. The Menopausal Transition: Analysis of LH, FSH, Estradiol, and Progesterone Concentrations During Menstrual Cycles of Older Women. (1976) https://doi.org/10.1210/jcem-42-4-629
10.
Burger, H. G. Diagnostic Role of Follicle-Stimulating Hormone (FSH) Measurements During the Menopausal Transition—An Analysis of FSH, Oestradiol and Inhibin. (1994) https://doi.org/10.1530/eje.0.1300038
11.
Burger, H. et al. The Endocrinology of the Menopausal Transition: a Cross-Sectional Study of a Population-Based Sample. (1995) https://doi.org/10.1210/jcem.80.12.8530596
12.
Harlow, S. et al. Executive Summary of the Stages of Reproductive Aging Workshop +10: Addressing the Unfinished Agenda of Staging Reproductive Aging. (2012) https://doi.org/10.1097/gme.0b013e31824d8f40
13.
Harlow, S. et al. Executive Summary of the Stages of Reproductive Aging Workshop +10: Addressing the Unfinished Agenda of Staging Reproductive Aging. (2012) https://doi.org/10.1016/j.fertnstert.2012.01.128
14.
Laine, C. et al. Menopause. (2009) https://doi.org/10.7326/0003-4819-150-7-200904070-01004
15.
Harper, J. et al. An Online Survey of Perimenopausal Women to Determine Their Attitudes and Knowledge of the Menopause. (2022) https://doi.org/10.1177/17455057221106890
16.
Gold, E. et al. Longitudinal Analysis of the Association Between Vasomotor Symptoms and Race/Ethnicity Across the Menopausal Transition: Study of Women’s Health Across the Nation. (2006) https://doi.org/10.2105/AJPH.2005.066936
17.
Woods, N. et al. Increased Urinary Cortisol Levels During the Menopause Transition. (2006) https://doi.org/10.1097/01.gme.0000198490.57242.2e
18.
Constantine, G. et al. Behaviours and Attitudes Influencing Treatment Decisions for Menopausal Symptoms in Five European Countries. (2016) https://doi.org/10.1177/2053369116632439
19.
Williams, R. E. et al. Healthcare seeking and treatment for menopausal symptoms in the United States. (2007) https://doi.org/10.1016/j.maturitas.2007.09.006
20.
Kling, J. M. et al. Menopause Management Knowledge in Postgraduate Family Medicine, Internal Medicine, and Obstetrics and Gynecology Residents: A Cross-Sectional Survey. (2018) https://doi.org/10.1016/j.mayocp.2018.08.033