Bone Health and Density: Why Menopause Is a Critical Time
Reading time 8 min

Reading time 8 min

When you think about menopause, you probably imagine hot flashes, mood swings, and sleepless nights. But there’s another silent change happening in your body that’s equally important but often overlooked: your bone health and density are quietly declining.
Why does menopause affect bone health and density?
Estrogen helps maintain the balance between bone breakdown and formation. When estrogen declines during menopause, this balance tips, leading to rapid bone loss and increased risk of osteoporosis.
Bone isn’t static. It’s living tissue that constantly renews itself through a process called bone remodeling. Imagine your bones as a construction site, with osteoclasts (the demolition crew) removing old bone and osteoblasts (the builders) laying down fresh, new bone. In younger years, estrogen helps keep this delicate balance in check.
But during perimenopause, things start to shift. Estrogen fluctuates and eventually drops sharply, leading to more demolition than construction. This imbalance speeds up dramatically after menopause, increasing the risk for conditions like osteopenia (early bone loss) and osteoporosis (severe bone loss).
As women move from premenopause into menopause, the rate of osteoporosis jumps significantly—from just 0.4% up to 12.7%, while osteopenia increases from 14.5% to 42.8%.
Research reveals that women can lose up to 20% of their lifetime bone density during the few years surrounding menopause. It depends on genetics and lifestyle. The spine, hips, and wrists (areas with spongier bone) are especially vulnerable.
That’s why fractures often appear first in these critical areas. Osteopenia is often not diagnosed or treated enough, especially in postmenopausal women, because it doesn’t show clear symptoms and has a lower risk of fractures compared to osteoporosis1, 2, 3, 4.
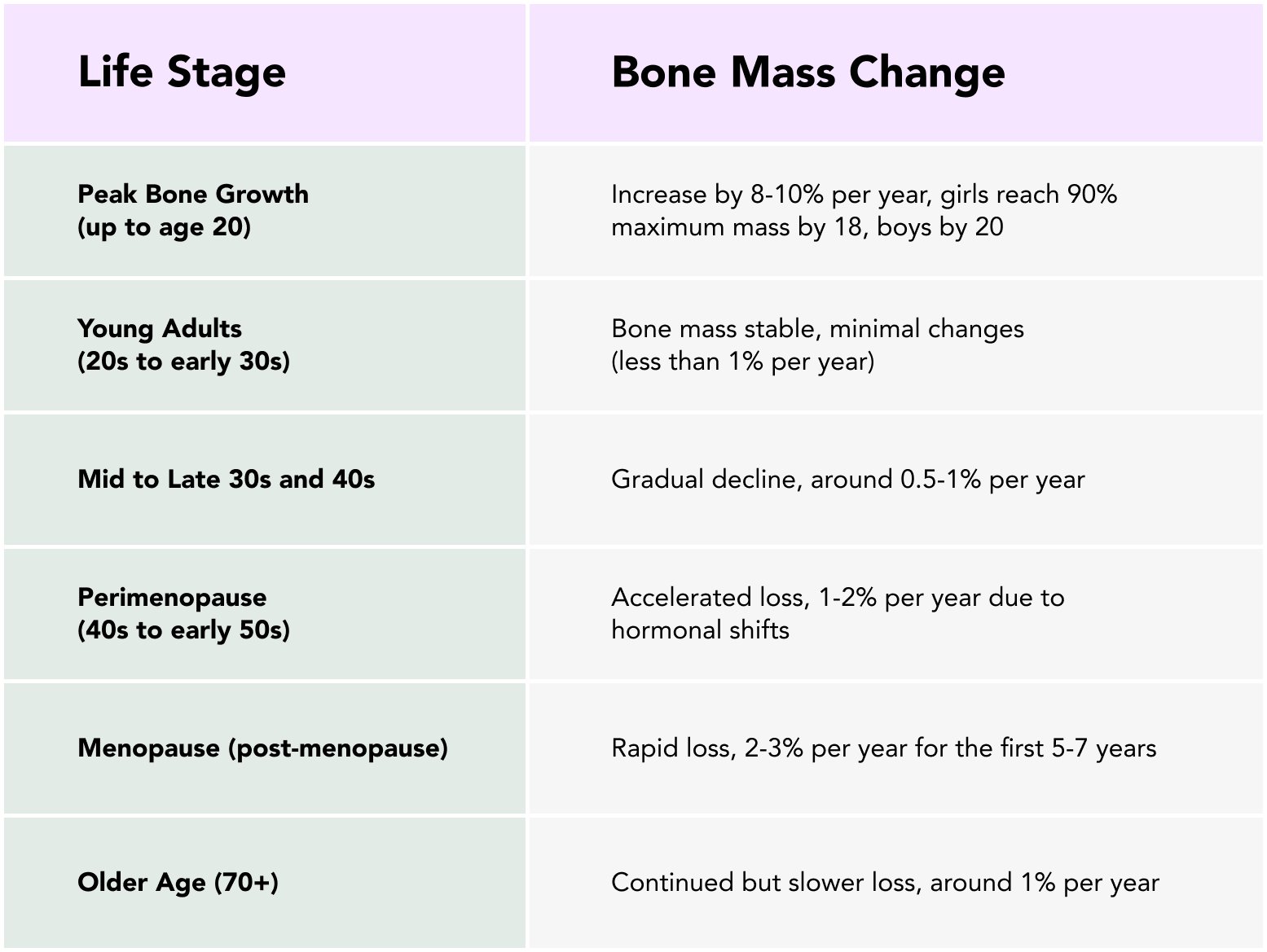
Bone is built when we are teenagers and lost when we hit our 40s12.
You might not even realize you’re losing bone density. There are typically no symptoms until a fracture occurs. That’s why testing is crucial5.
The gold standard, a painless, low-radiation test that measures your bone mineral density (BMD) at key sites (hip and spine). It’s simple, quick, and crucial for identifying osteopenia and osteoporosis.
Quick screenings at the heel or wrist are less precise but good initial indicators if further DXA testing is needed.
Blood and urine tests provide insights into how quickly your bones are breaking down and rebuilding.
The good news is that you have significant control over your bone health. Here’s what science says works6, 7, 8.
Aim for 1000-2000 mg/day. Sources include dairy products, fortified plant-based milks, leafy greens, and calcium supplements.
Aim for a minimum of 800–1000 IU/day of Vitamin D. Sources include fatty fish, fortified foods, and sunlight.
Vitamin C seems to work in synergy with Calcium to prevent/slow down bone loss. Studies suggest that the minimum you should take is 95-100 mg/day while some suggest up to 5000mg/day.

Regular weight-bearing exercises (brisk walking, jogging, dancing) and muscle-strengthening workouts (resistance training) dramatically slow bone loss. Consistency is key! Lean body mass (muscle), rather than fat mass, plays a crucial role in maintaining bone mineral density (BMD). Start lifting heavy, ladies!
Quit smoking, limit alcohol, and maintain a healthy weight. Underweight women lose bone faster, while moderate body weight protects bone density.
Make your environment safer, improve lighting, remove tripping hazards, and practice balance exercises like tai chi or yoga.
Increasing estrogen can prevent the rapid bone loss around perimenopause and significantly reduce fracture risk while it’s used.
If you’ve been diagnosed with osteopenia or osteoporosis, treatment options can significantly improve bone density and reduce fracture risks. Generally, these medical treatments fall into two categories: anabolic therapies that build new bone, and antiresorptive therapies that slow down bone loss9, 10, 11.
Medications like alendronate (Fosamax) and risedronate (Actonel) reduce bone breakdown and help maintain bone density.
Effective especially during early menopause, HRT can help maintain bone density by supplementing estrogen levels.
Drugs like raloxifene (Evista) have estrogen-like effects beneficial for bones without affecting other tissues.
A monoclonal antibody administered by injection every six months, significantly reducing bone resorption.
Treatments like teriparatide (Forteo) and abaloparatide (Tymlos) stimulate new bone formation, beneficial for severe cases.
Always consult your healthcare provider to determine the most appropriate treatment based on your specific health needs and conditions.
Bone health might not feel urgent. Until it suddenly is. Understanding the changes your bones go through during menopause can empower you to take charge. Starting early with preventive measures like staying active, eating calcium-rich foods, and keeping up with regular screenings, makes a huge difference.
I strongly believe that early testing is essential because preventing bone loss is always easier and more effective than treating it after the fact. Remember, menopause is inevitable, but significant bone loss doesn’t have to be. Stay strong, informed, and proactive. Your future self will thank you.
Dr. Jura Lasas
1.
Noirrit-Esclassan, E. et al. Critical Role of Estrogens on Bone Homeostasis in Both Male and Female: From Physiology to Medical Implications. (2021) https://doi.org/10.3390/ijms22041568
2.
Santos, L. et al. Exercise and bone health across the lifespan. (2017) https://doi.org/10.1007/s10522-017-9732-6
3.
Shariati-Sarabi, Z. et al. Evaluation of Bone Mineral Density in Perimenopausal Period. (2018) https://doi.org/10.22038/abjs.2017.19433.1506
4.
Simon, James. Does osteopenia warrant treatment? (2005) https://doi.org/10.1097/01.GME.0000156346.77014.FB
5.
Blake, B. et al. The role of DXA bone density scans in the diagnosis and treatment of osteoporosis. (2007) https://doi.org/10.1136/pgmj.2007.057505
6.
Tu, K. et al. Osteoporosis: A Review of Treatment Options. (2018) http://www.ncbi.nlm.nih.gov/pmc/articles/pmc5768298/
7.
Ahmadieh, H. et al. Vitamins and bone health: beyond calcium and vitamin D. (2011) https://doi.org/10.1111/j.1753-4887.2011.00372.x
8.
Heaney, R. Chapter 27 – Nutrition and Risk for Osteoporosis. (2001) https://www.sciencedirect.com/science/article/abs/pii/B9780124708624500283?via%3Dihub
9.
Karaguzel, G. et al. Diagnosis and treatment of osteopenia. (2011) https://link.springer.com/article/10.1007/s11154-010-9154-0
10.
Chen, J. et al. Antiresorptive therapies for osteoporosis: a clinical overview. (2012) https://doi.org/10.1038/nrendo.2011.146
11.
Stapleton, M. et al. Development of Bone Targeting Drugs. (2017) https://doi.org/10.3390/ijms18071345
12.
Faienza, M. et al. How Physical Activity across the Lifespan Can Reduce the Impact of Bone Ageing: A Literature Review. (2020) https://doi.org/10.3390/ijerph17061862