Hormonal Changes During Menopause: Get to Know Your 7 Allies
Reading time 11 min

Reading time 11 min

Ever feel like your body has been taken over by a rollercoaster of changes? One day, you’re cool as a cucumber; the next, you debate the merits of installing a personal walk-in freezer. Your sleep schedule is gone, leaving you staring at the ceiling at 3 AM, contemplating the meaning of life. And let’s not even talk about how your trusty vocabulary has suddenly decided to play hide-and-seek, leaving you grasping for words mid-sentence.
It’s not your imagination! These shifts are largely driven by hormonal changes during menopause – the powerful chemical messengers affecting your energy, mood, sleep, and even your memory, often without warning.
What are the hormonal changes during menopause?
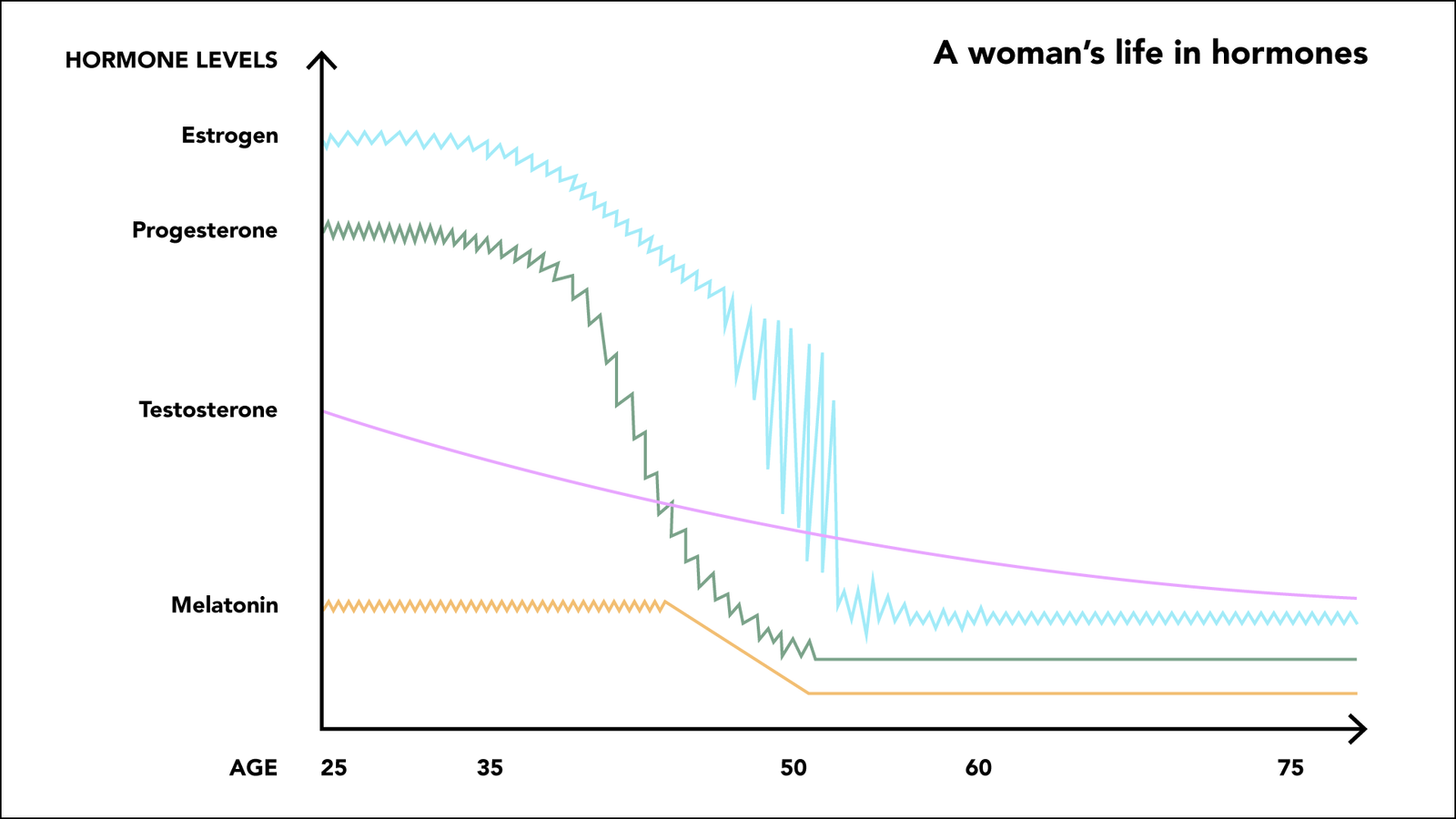
Hormonal changes during menopause include declines in estrogen, progesterone, and testosterone, with increases in FSH and LH. These shifts drive symptoms like hot flashes, mood swings, bone loss, and more.
But what if you could decode these changes and make them work for you?
Meet the seven hormonal allies that will help you better understand the menopause transition.
Did you know that estrogen affects almost every organ in your body? Estrogen is like your inner superpower, constantly working to keep your body functioning smoothly, from supporting your brain health to maintaining strong bones. It’s much more than just a hormone for reproduction; it plays a vital role in your overall well-being. Estrogen works by attaching to specific proteins, called receptors (like tiny locks) in your body’s cells10, 11, 12.
When estrogen binds to these receptors, it “unlocks” the cells, telling them what to do:
Estrogen Receptors Alpha (ERα) are found mainly in your reproductive organs, breasts, liver, and brain. They are involved in growth and reproductive functions10.
Estrogen Receptors Beta (ERβ) are found in the ovaries, lungs, digestive system, and brain. These receptors help control inflammation and balance the effects of ERα. While ERα promotes cell growth, ERβ acts as a counterbalance, slowing down excessive growth and helping to regulate healthy cell function11.
As estrogen levels drop, these receptors aren’t activated as much, leading to symptoms like weaker bones and changes in how your body processes food and energy13. Understanding these changes can empower you to handle your symptoms better and make informed decisions about your health.
Understanding the three types of estrogen – estradiol (E2), estrone (E1), and estriol (E3) – is key to navigating hormonal shifts during midlife. Each form plays a unique role in your body, and their balance changes significantly before, during, and after menopause. These changes don’t just affect your reproductive system – they influence everything from mood to metabolism1, 2, 3.
Estradiol (E2)
This is the strongest and most common form of estrogen before menopause. It’s mainly produced by your ovaries and regulates your menstrual cycle while supporting your reproductive health. As you get closer to perimenopause, your levels of estradiol start to go up and down, causing symptoms like hot flashes and mood swings4, 5, 6.
Estrone (E1)
After menopause, estrone becomes the main form of estrogen in your body. Fat tissue becomes a significant source of estrone7, as it’s made in fat tissue, the ovaries, and the adrenal glands. Estrone can convert into estradiol when needed, but high levels of estrone after menopause are linked to a higher risk of breast cancer. Monitoring estrone levels can help in assessing this risk7, 8, 9.
Estriol (E3)
This is the weakest form of estrogen and is mostly produced during pregnancy3.
Let’s break down what happens in your body each month, step by step.
Step 1 – in the first half of your menstrual cycle, eggs start to develop and mature in follicles, which are like tiny nests. As the follicles grow, they produce estrogen, which prompts your body to begin preparing the uterine lining by making it thicker, like creating a soft landing place in case a fertilized egg needs to implant.
Step 2 – when the egg is fully mature, estrogen levels reach the peak. High estrogen levels send a signal to your brain to release Luteinizing Hormone (LH). This hormone acts like a green light, triggering ovulation, where the egg leaves its follicle and starts its journey down the fallopian tube. The empty follicle starts producing progesterone.
Step 3 – if the egg isn’t fertilized, estrogen and progesterone levels drop. These hormones are essential for maintaining the uterine lining, and without them, the lining begins to break down. The broken down lining is expelled as menstrual bleeding.
Changes that you experience during perimenopause and menopause are largely due to fluctuating estrogen levels. These fluctuations can lead to noticeable physical and emotional symptoms. Hot flashes, night sweats, and sleep disturbances can become unwelcome bedfellows. Your skin and vagina might feel drier, while your waistline decides to expand without you changing anything. Energy levels can resemble a roller coaster, and your emotions might surprise you with their intensity. The changes are real, but you do not have to be helpless. You can take control and apply the different tools that we provide.
Think of progesterone as your body’s balancing hormone, essential for keeping your menstrual cycle regular and preparing you for pregnancy. After ovulation (when the egg leaves its follicle and starts its journey down the fallopian tube), progesterone works behind the scenes to stabilize the uterine lining, maintaining harmony in the delicate dance between estrogen and your reproductive system14.
As you enter perimenopause, progesterone levels start to drop because ovulation becomes more irregular15. Without enough progesterone, the balance is thrown off, and you may notice some changes – your periods might become heavier, longer, or more unpredictable. Due to the lower levels of progesterone, you may also experience symptoms like mood swings, sleep disturbances, or breast tenderness.
In addition, progesterone normally prevents estrogen from overstimulating the uterine lining. When progesterone is low, estrogen can lead to excessive growth of the uterine lining, increasing the risk of cancer16.
Even though it’s often thought of as a “male” hormone, it’s vital for women’s overall health. It helps keep your muscles strong, boosts your energy, and plays a role in your sex drive.
During perimenopause and menopause, testosterone levels slowly decline. This can cause changes like a lower sex drive, less natural moisture in the vagina, and a decrease in muscle tone20, 21, 4. Interestingly, as estrogen levels drop more quickly, the balance between testosterone and estrogen shifts. This can lead to what’s known as androgen excess, where you might notice signs like acne or unwanted hair growth on the face22.
“Noticing those thick hairs on your chin? That’s one of the effects of this testosterone and estrogen shift.”
Did you know that cholesterol is essential for several important functions in your body? Estrogen, progesterone, and testosterone are all made from cholesterol, primarily in the ovaries and adrenal glands26. Cholesterol acts as a building block for bile acids (which help digest fats in the small intestine), steroid hormones (such as estrogen, progesterone, testosterone, cortisol), and vitamin D27. It also plays a vital role in maintaining the structure and flexibility of cell walls, ensuring your cells function properly.
Cholesterol itself isn’t “bad”. Your body gets cholesterol from your diet and from making it in the liver. Even after menopause, your body continues to produce cholesterol in the same way as before menopause. However, as estrogen levels decline during perimenopause and postmenopause, the way your body handles cholesterol changes increasing the risk of heart disease.
Follicle-Stimulating Hormone (FSH) is the signal from your brain that helps your ovaries prepare for ovulation each month. Produced by the pituitary gland (which is like the body’s master conductor directing the hormonal orchestra), FSH stimulates the growth of ovarian follicles – the small nests in your ovaries that hold immature eggs17.
As you approach perimenopause and menopause, your estrogen levels decline, and your ovaries become less responsive to FSH. To compensate, your brain produces higher levels of FSH, trying to stimulate the ovaries to release eggs. This increase in FSH is one of the body’s ways of signaling that you’re approaching menopause18, 19. High FSH levels are often used as a marker to determine where you are in the menopausal transition. It is relatively easy to have your FSH levels measured by a doctor through a simple blood test.
However, it’s important to note that FSH levels fluctuate throughout the menstrual cycle, even during perimenopause, so a single test may not always provide a definitive result28, 32. Higher FSH levels may increase the risk of heart disease after menopause31. High FSH levels could also affect cognitive function (thinking and memory)30. More research is needed to fully understand this connection in women29.
Luteinizing Hormone (LH) is the key hormone that triggers ovulation, the release of an egg from the follicle. LH also supports the production of estrogen and progesterone after ovulation, helping to maintain a healthy menstrual cycle. Low levels of LH can cause cycles where no ovulation occurs. This can make pregnancy difficult and lead to hormonal imbalances, causing irregular periods.
As you enter perimenopause and your ovaries become less responsive, they produce less estrogen and progesterone. In response, LH levels rise, similar to FSH levels. This is your body’s way of trying to stimulate the ovaries. Once you reach menopause and ovulation stops completely, LH levels remain elevated since the ovaries no longer produce significant amounts of estrogen and progesterone22.
Evidence from animal studies and large-population (epidemiological) research suggests that elevated LH levels may contribute to age-related cognitive decline. Some studies also indicate a possible connection between high LH levels and an increased risk of Alzheimer’s disease33, 34, 35. There might be associations between high LH levels and problems like bone loss, muscle weakening, and metabolic disturbances, but more research is needed to fully understand these links.
Anti-Müllerian Hormone (AMH) is produced by the follicles. AMH levels show how many viable eggs you have left. As you approach menopause, AMH levels decline because the number of follicles decreases over time. This drop in AMH reflects the shrinking supply of eggs, signaling that your ovaries are nearing the end of their reproductive phase24.
AMH is often used to gauge how close you are to menopause, helping you understand where you are in this transition. It’s done through a simple blood test. Unlike some other hormones, AMH levels remain fairly stable throughout your menstrual cycle, which means the test can be taken at any time.
Recent research shows that lower levels of AMH during perimenopause are associated with an increased chance of experiencing vasomotor symptoms (VMS), such as hot flashes and night sweats, after menopause36. One article has also shown that lower AMH levels during perimenopause are linked to a higher risk of heart disease after menopause37.
Inhibins (Inhibin A and Inhibin B) are hormones produced by the follicles. Their main job is to regulate Follicle-Stimulating Hormone (FSH) production, helping to maintain hormonal balance25. As the number of follicles decreases during perimenopause, the levels of Inhibin A and B begin to drop. With fewer inhibins around to regulate FSH, FSH levels rise, contributing to the hormonal shifts you experience during the transition to menopause. Also, falling levels of inhibins during perimenopause are linked to increased bone breakdown38.
Navigating the hormonal shifts of perimenopause and postmenopause can feel overwhelming. The period of transition is characterized by significant fluctuations in hormones, particularly estrogen. Now, you’ve met your seven allies – the architects of your energy, mood, and physical changes. Estrogen is the most powerful of them all. It affects almost every organ in your body, supporting functions like bone strength, brain health, and metabolism. As estrogen levels decline, you start to experience symptoms like weaker bones, mood swings, and changes in energy levels.
In addition, the balance with other hormones like FSH, progesterone, or LH changes. It means more symptoms that can feel unpredictable and hard to manage.
I find it empowering to understand the biological reasons for the changes that are taking place in our bodies. After all, cognitive behavioral therapy is based on understanding the underlying patterns and beliefs of feelings or behaviors we might want to change. Remember, knowledge isn’t just about managing symptoms – it’s about gaining back the quality and control of your life.
Dr. Jūra Lašas
1.
Nelson, L. et al. Estrogen production and action. (2001) https://doi.org/10.1067/mjd.2001.117432
2.
Simpson, E. Sources of estrogen and their importance. (2003) https://doi.org/10.1016/S0960-0760(03)00360-1
3.
Nelson, L. et al. Sources of estrogen and their importance. (2001) https://doi.org/10.1067/mjd.2001.117432
4.
Burger, H. et al. Hormonal Changes in the Menopause Transition. (2002) https://doi.org/10.1210/RP.57.1.257
5.
Shideler, S. et al. Ovarian-pituitary hormone interactions during the perimenopause. (1989) https://doi.org/10.1016/0378-5122(89)90029-7
6.
Burger, H. et al. Cycle and hormone changes during perimenopause the key role of ovarian function. (2008) https://doi.org/10.1097/gme.0b013e318174ea4d
7.
Suzuki, N. et al. A possible role of estrone produced in adipose tissues in modulating postmenopausal bone density. (1995) https://doi.org/10.1016/0378-5122(95)00902-W
8.
Lu, L. et al. Postmenopausal osteoporosis coexisting with sarcopenia: the role and mechanisms of estrogen. (2023) https://doi.org/10.1530/JOE-23-0116
9.
Qureshi, R. et al. The Major Pre- and Postmenopausal Estrogens Play Opposing Roles in Obesity-Driven Mammary Inflammation and Breast Cancer Development. (2020) https://doi.org/10.1016/j.cmet.2020.05.008
10.
Tang, Z. et al. Estrogen-Receptor Expression and Function in Female Reproductive Disease. (2019) https://doi.org/10.3390/cells8101123
11.
Hapangama, D. et al. Estrogen receptor β: the guardian of the endometrium. (2014) https://doi.org/10.1093/humupd/dmu053
12.
Fuentes, N. et al. Chapter Three – Estrogen receptor signaling mechanisms. (2019) https://doi.org/10.1016/BS.APCSB.2019.01.001
13.
Dey, P. et al. Insight into the mechanisms of action of estrogen receptor β in the breast, prostate, colon, and CNS. (2013) https://doi.org/10.1530/JME-13-0150
14.
Patel, B. et al. Role of nuclear progesterone receptor isoforms in uterine pathophysiology. (2014) https://doi.org/10.1093/humupd/dmu056
15.
Jewson, M. et al. Progesterone and abnormal uterine bleeding/menstrual disorders. (2020) https://doi.org/10.1016/j.bpobgyn.2020.05.004
16.
Kolatorova, L. et al. Progesterone: A Steroid with Wide Range of Effects in Physiology as Well as Human Medicine. (2022) https://doi.org/10.3390/ijms23147989
17.
Sherman, B. et al. The Menopausal Transition: Analysis of LH, FSH, Estradiol, and Progesterone Concentrations During Menstrual Cycles of Older Women. (1976) https://doi.org/10.1210/JCEM-42-4-629
18.
Burger, H. Diagnostic role of follicle-stimulating hormone (FSH) measurements during the menopausal transition—an analysis of FSH, oestradiol and inhibin. (1994) https://doi.org/10.1530/EJE.0.1300038
19.
Burger, H. et al. The endocrinology of the menopausal transition: a cross-sectional study of a population-based sample. (1995) https://doi.org/10.1210/JCEM.80.12.8530596
20.
Scott, A. et al. Should we be prescribing testosterone to perimenopausal and menopausal women? A guide to prescribing testosterone for women in primary care. (2020) https://doi.org/10.3399/bjgp20X709265
21.
Schwenkhagen, A. Hormonal Changes in Menopause and Implications on Sexual Health. (2007) https://doi.org/10.1111/J.1743-6109.2007.00448.X
22.
Torréns, J. et al. Relative androgen excess during the menopausal transition predicts incident metabolic syndrome in midlife women; Study of Women’s Health Across the Nation. (2009) https://doi.org/10.1097/gme.0b013e318185e249
23.
Hale, G. et al. Endocrine Features of Menstrual Cycles in Middle and Late Reproductive Age and the Menopausal Transition Classified According to the Staging of Reproductive Aging Workshop (STRAW) Staging System. (2007) https://doi.org/10.1210/jc.2007-0066
24.
Sowers, M. et al. Anti-Mullerian Hormone and Inhibin B in the Definition of Ovarian Aging and the Menopause Transition. (2008) https://doi.org/10.1210/jc.2008-0567
25.
Iwahashi, M. et al. Decreased Type III and V Collagen Expression in Chorionic Villi of Hydatidiform Mole. (2001) https://doi.org/10.1210/jcem.86.7.7632
26.
Miller, W. et al. Early steps in steroidogenesis: intracellular cholesterol trafficking. (2011) https://doi.org/10.1194/jlr.R016675
27.
Luo, J. et al. Mechanisms and regulation of cholesterol homeostasis. (2020) https://doi.org/10.1038/s41580-019-0190-7
28.
Burger, H. Diagnostic role of follicle-stimulating hormone (FSH) measurements during the menopausal transition—an analysis of FSH, oestradiol and inhibin. (1994) https://doi.org/10.1530/EJE.0.1300038
29.
Khoudary, S. Gaps, limitations and new insights on endogenous estrogen and follicle stimulating hormone as related to risk of cardiovascular disease in women traversing the menopause: A narrative review. (2017) https://doi.org/10.1016/J.MATURITAS.2017.08.003
30.
Mao, L. et al. Effects of follicle-stimulating hormone on fat metabolism and cognitive impairment in women during menopause. (2022) https://doi.org/10.3389/fphys.2022.1043237
31.
Song, Y. et al. Follicle-Stimulating Hormone Induces Postmenopausal Dyslipidemia Through Inhibiting Hepatic Cholesterol Metabolism. (2016) https://doi.org/10.1210/jc.2015-2724
32.
Burger, H. Diagnostic role of follicle-stimulating hormone (FSH) measurements during the menopausal transition—an analysis of FSH, oestradiol and inhibin. (1994) https://doi.org/10.1530/EJE.0.1300038
33.
Mey, M. et al. Luteinizing hormone and the aging brain. (2021) https://doi.org/10.1016/bs.vh.2020.12.005
34.
Burnham, V. et al. Luteinizing hormone as a key player in the cognitive decline of Alzheimer’s disease. (2015) https://doi.org/10.1016/j.yhbeh.2015.05.010
35.
Bhatta, S. et al. Luteinizing Hormone Involvement in Aging Female Cognition: Not All Is Estrogen Loss. (2018) https://doi.org/10.3389/fendo.2018.00544
36.
NamGoung, S. et al. Low anti-Müllerian hormone levels are associated with an increased risk of incident early-onset vasomotor symptoms among premenopausal women. (2022) https://doi.org/10.1038/s41598-022-16182-7
37.
El Khoudary, S. et al. The independent associations of anti-Müllerian hormone and estradiol levels over the menopause transition with lipids/lipoproteins: The Study of Women’s health Across the Nation. (2023) https://doi.org/10.1016/j.jacl.2022.11.008
38.
Perrien, D. et al. Bone turnover across the menopause transition: correlations with inhibins and follicle-stimulating hormone. (2006) https://doi.org/10.1210/JC.2005-2423