Your Ultimate Guide to Hormone Replacement Therapy: Which Type Works Best for You?
Reading time 10 min
Reading time 10 min
Pills, patches, gels – it’s easy to get overwhelmed by the different hormone replacement therapy types available. Each method works differently and suits different needs. This guide explains your options so you can match your symptoms, preferences, and lifestyle with the HRT that works best for you.
What are the different hormone replacement therapy types?
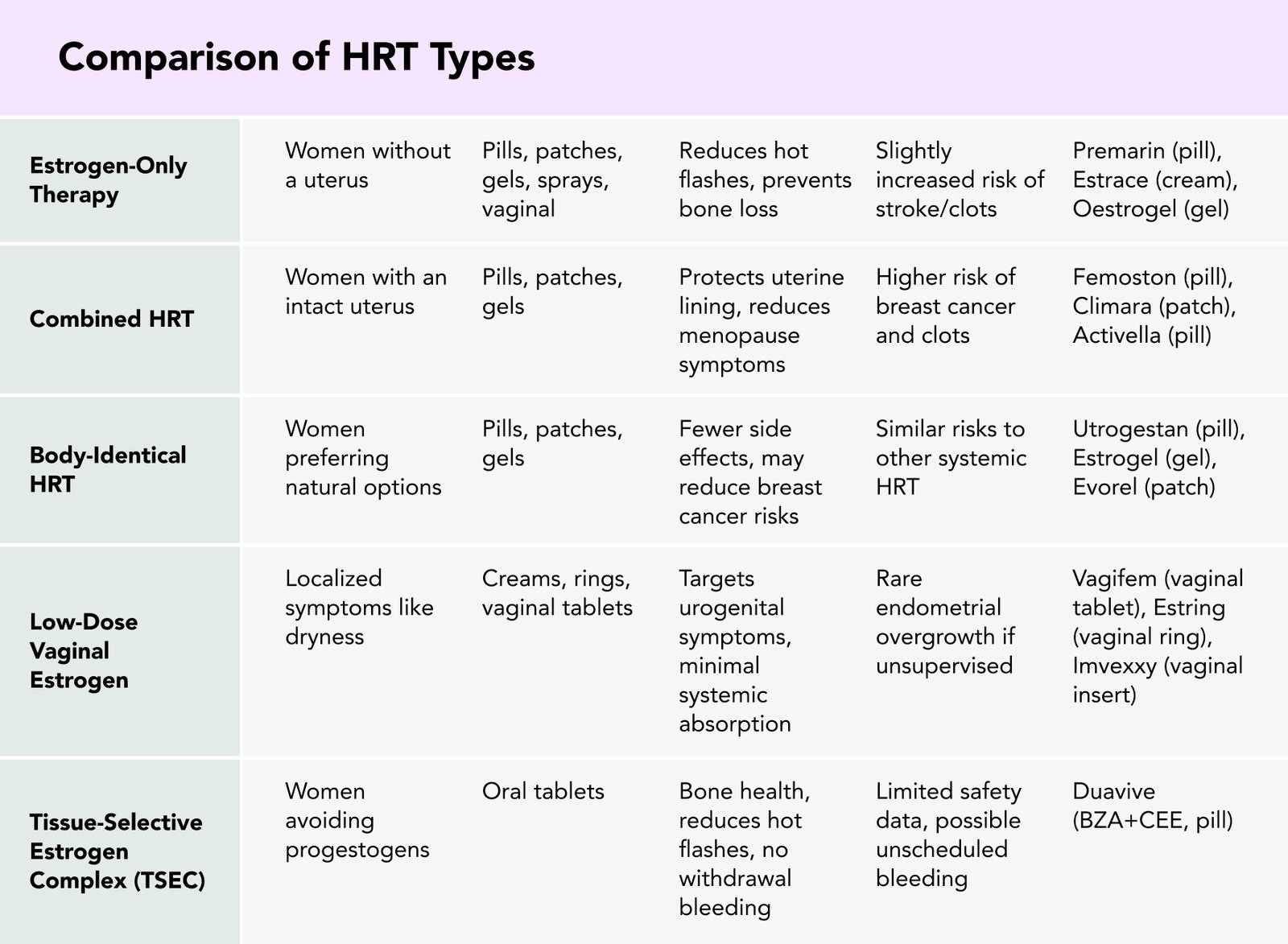
Hormone replacement therapy types include estrogen-only therapy, combined HRT, body-identical HRT, low-dose vaginal estrogen, and newer options like TSEC and Tibolone. Each type differs in its benefits, risks, and delivery method. Your choice depends on your symptoms, medical history, and personal preference – always consult your doctor first.
HRT can help alleviate the following common menopause symptoms1, 3:
As discussed throughout my articles, it can also help alleviate lesser-known symptoms. Always consult with your doctor before making any decisions – their guidance is key to finding a safe and effective option for you2.
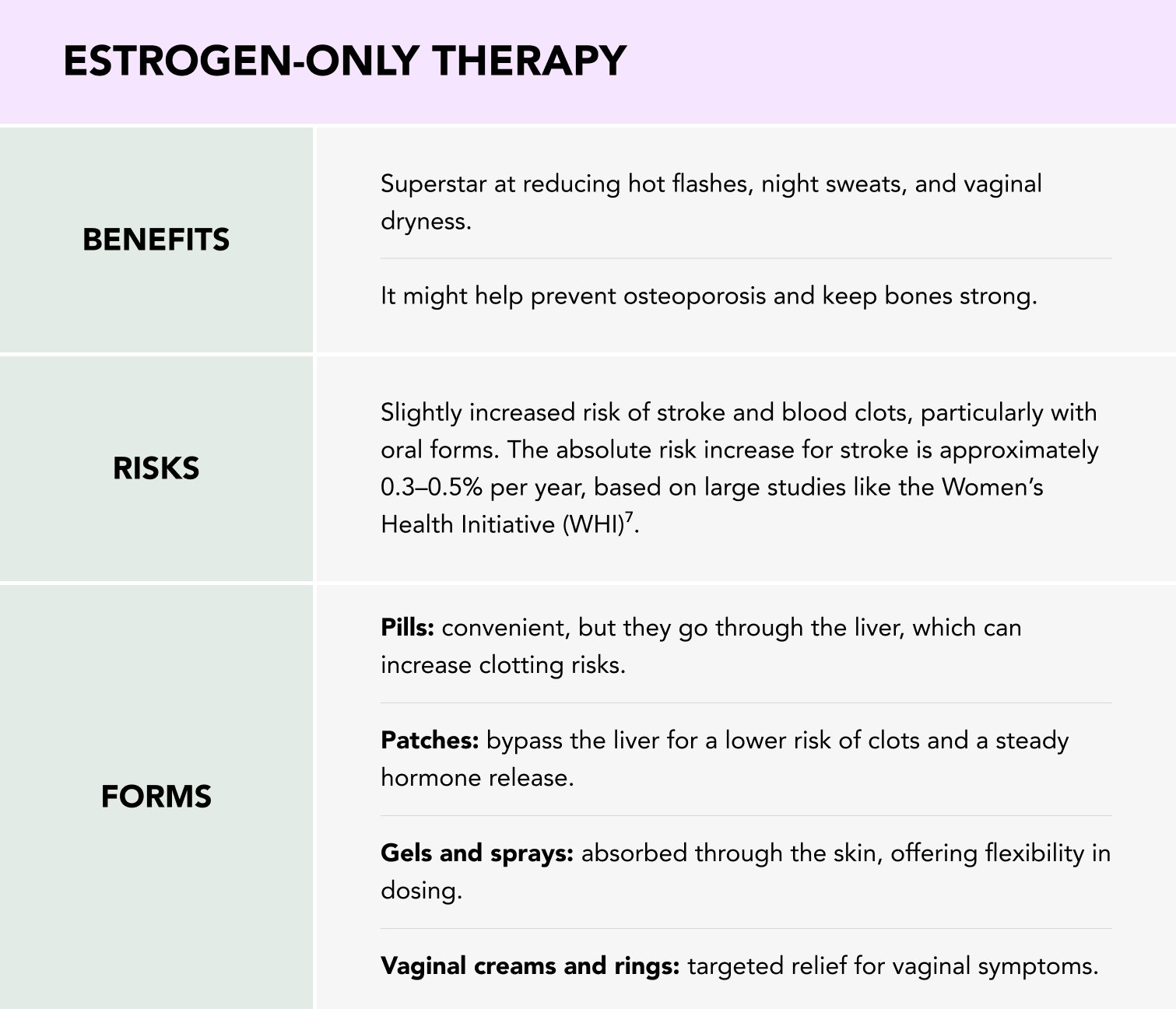
If you’ve had a hysterectomy, estrogen-only therapy is likely your best option. Without a uterus, there’s no risk of estrogen-induced endometrial cancer, so no need for progesterone to counterbalance the estrogen. Progesterone is essential for women with a uterus because it prevents the overgrowth of the uterine lining, which can lead to endometrial cancer4, 6.
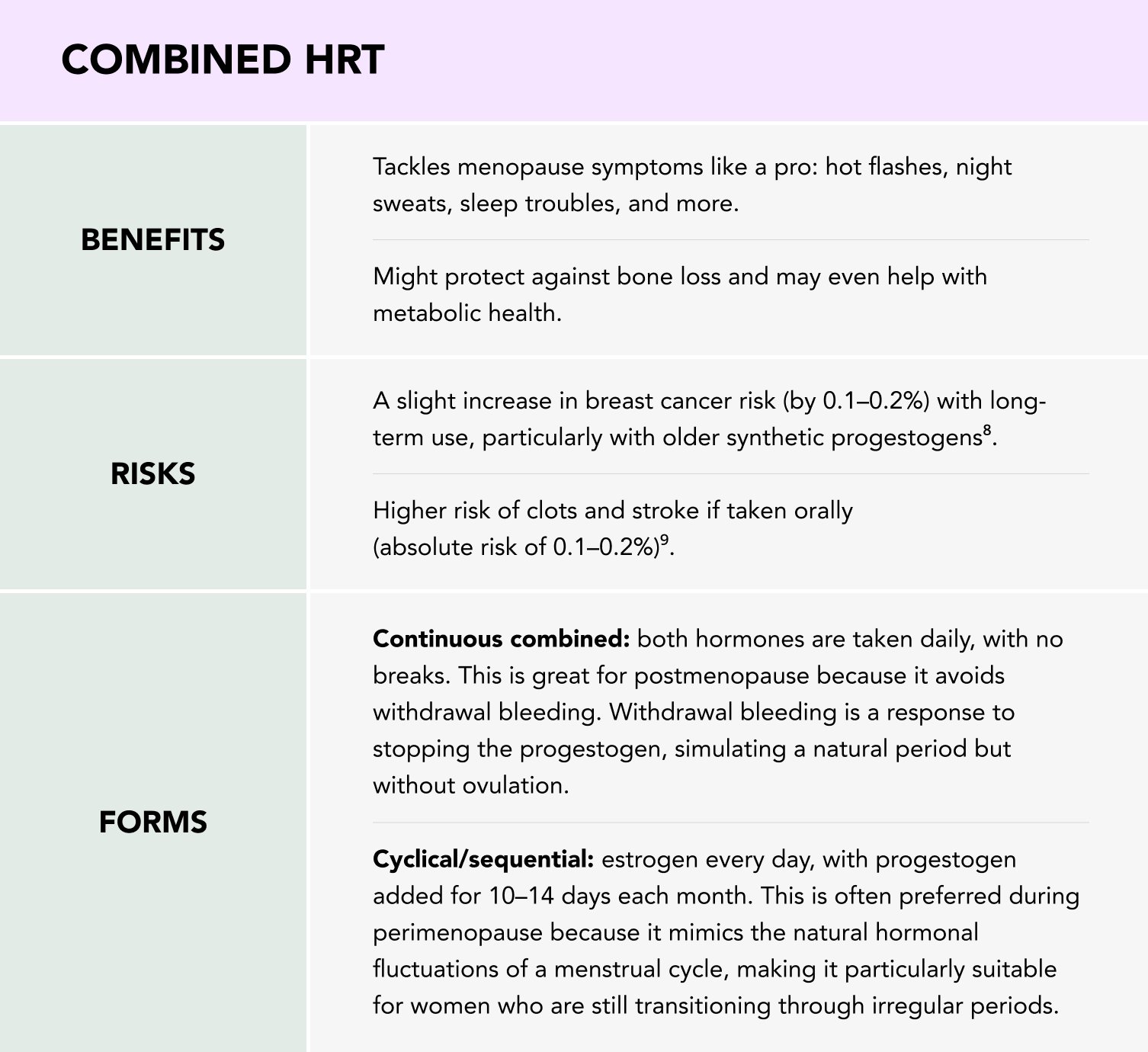
If you still have your uterus, you’ll need combined HRT – a mix of estrogen and progestogen – to protect your uterine lining from overgrowth caused by estrogen alone. Estrogen stimulates the growth of the uterine lining, and without progesterone, this overgrowth can increase the risk of endometrial cancer. Using both hormones together creates a balance, ensuring the benefits of estrogen without its associated risks to the uterus5, 6.
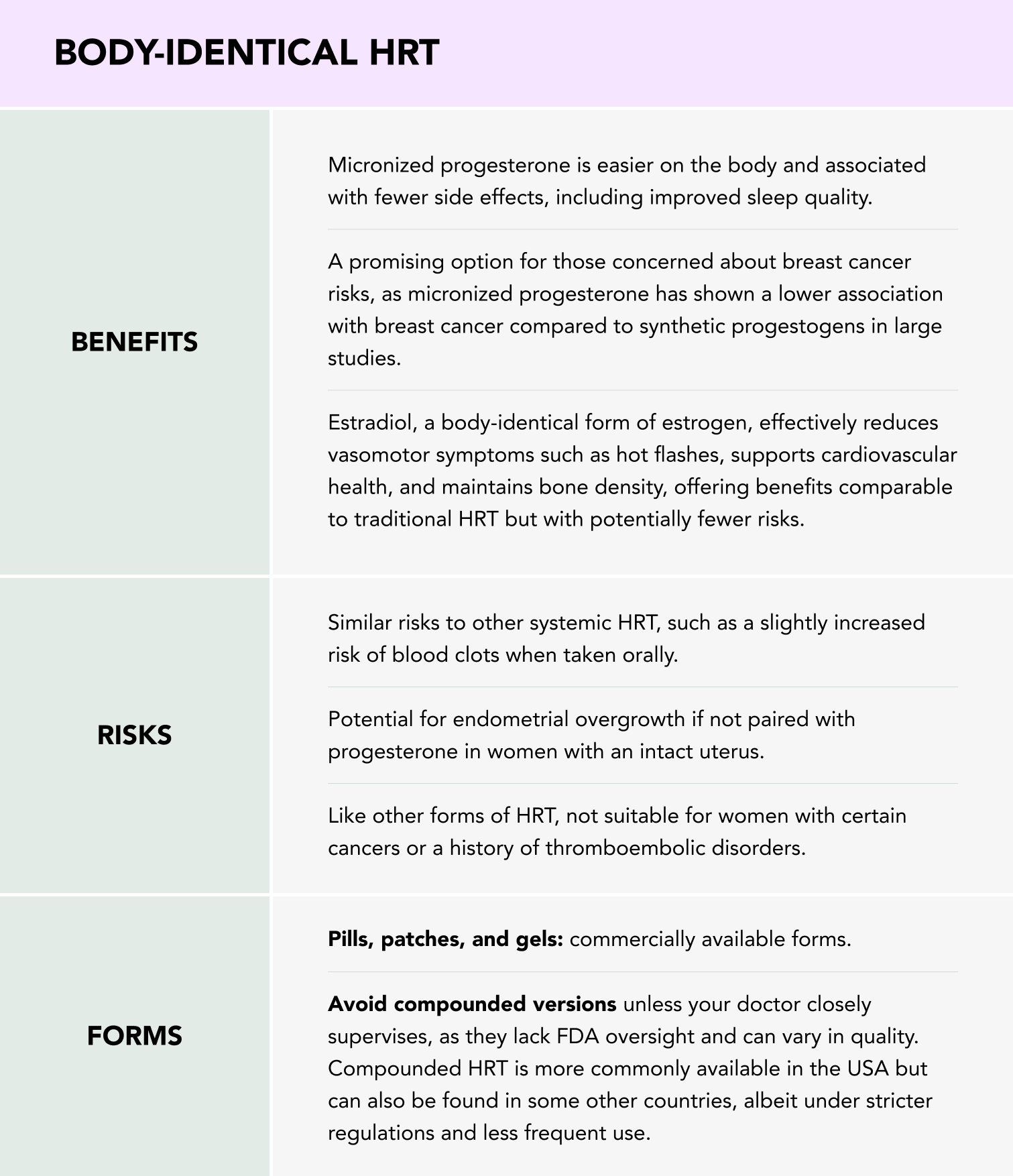
Body-identical HRTs are chemically identical to what your body produces. This includes both estrogen (like estradiol) and progesterone (like micronized progesterone), offering a more natural alignment with the body’s hormonal balance. These aren’t to be confused with compounded bioidenticals (which we discuss here)10.
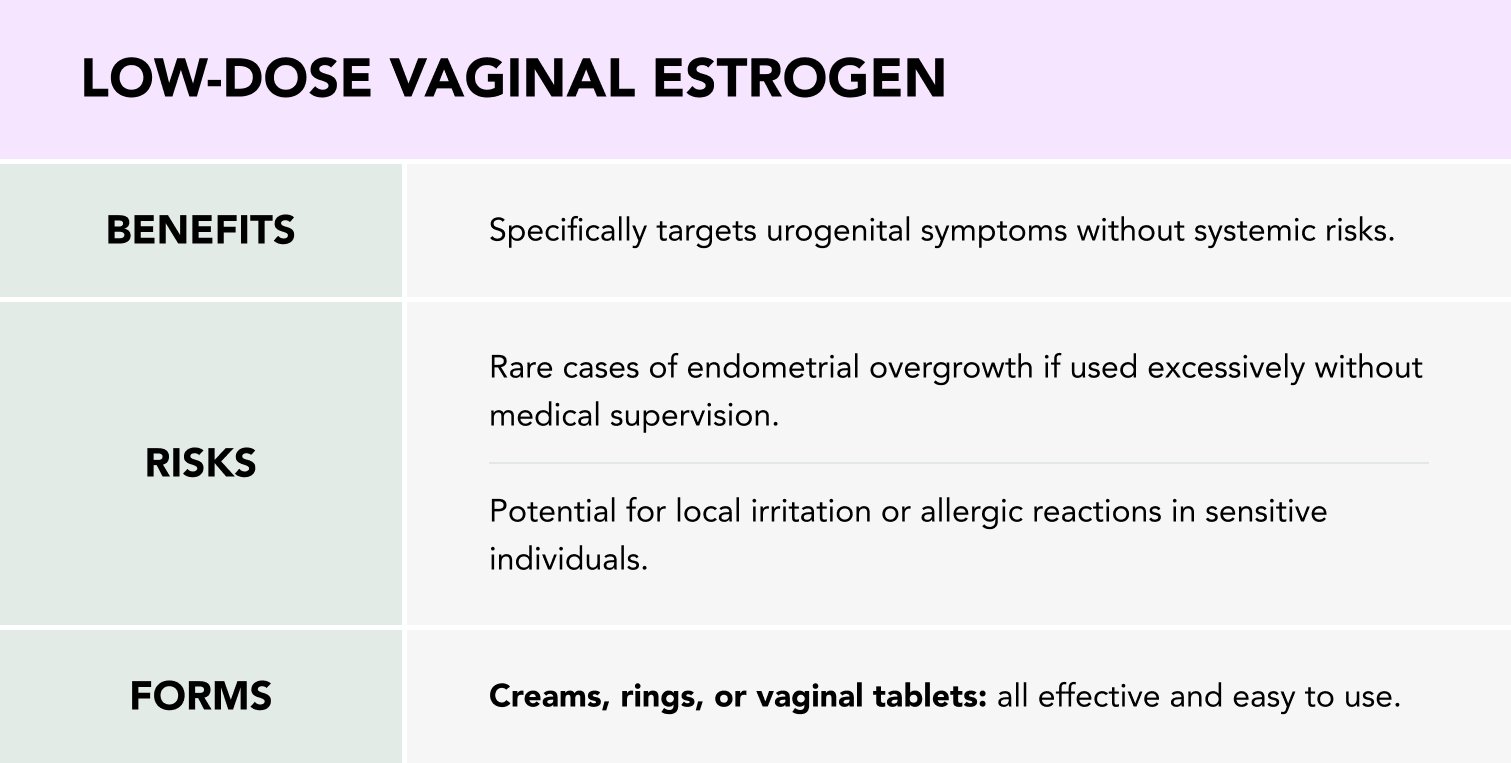
For vaginal dryness, discomfort during sex, or mild urinary issues, low-dose vaginal estrogen is a game-changer. It’s hyper-local, so there’s minimal absorption into the bloodstream. This localized approach minimizes systemic risks, making it a safe option even for women who cannot use systemic estrogen therapy11.
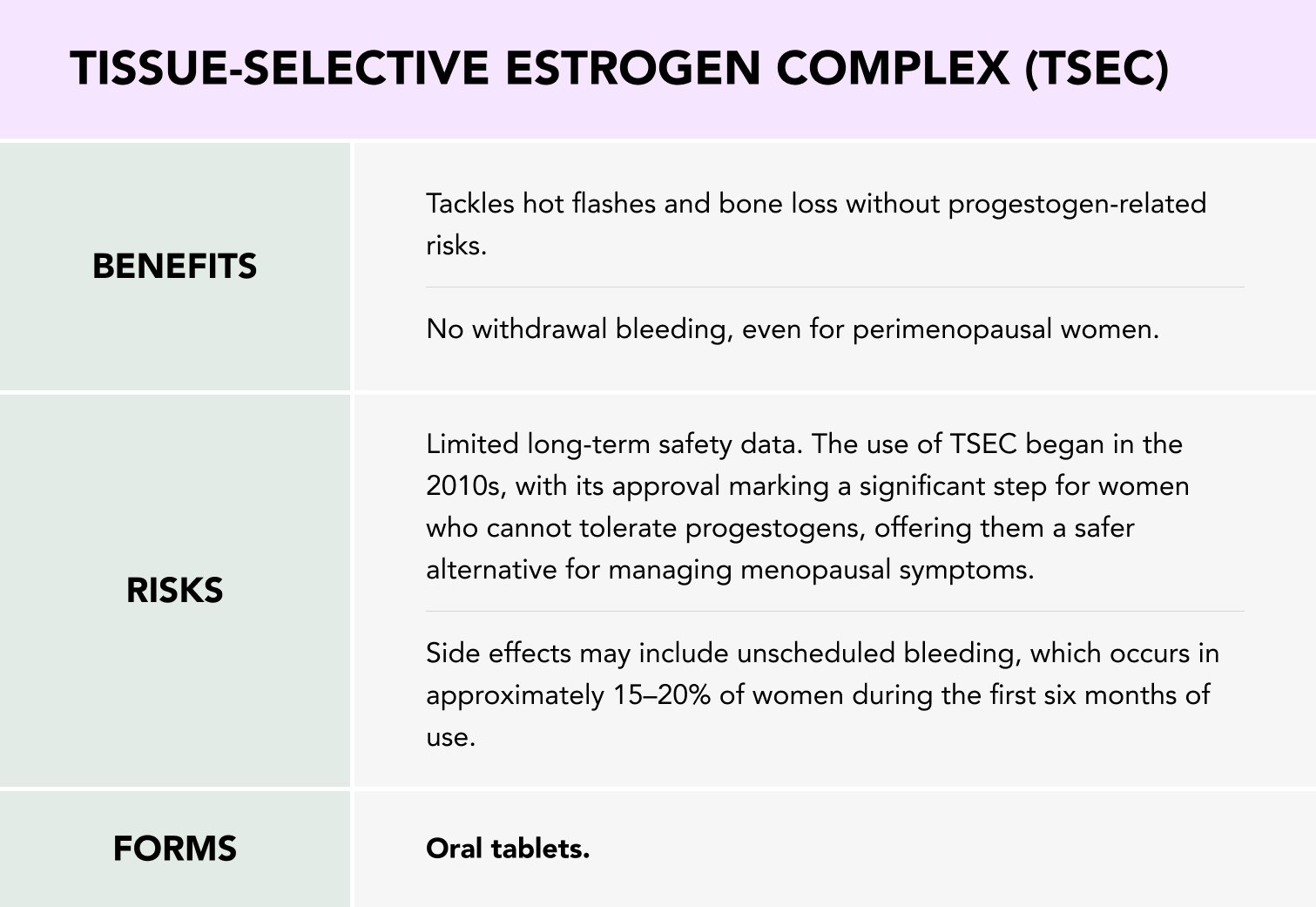
This combines estrogen with a selective estrogen receptor modulator (SERM) like bazedoxifene. Think of it as estrogen with built-in protection for your uterus, meaning no need for added progestogen. SERM is particularly useful for women who cannot tolerate progesterone or have a history of progesterone-related side effects12.
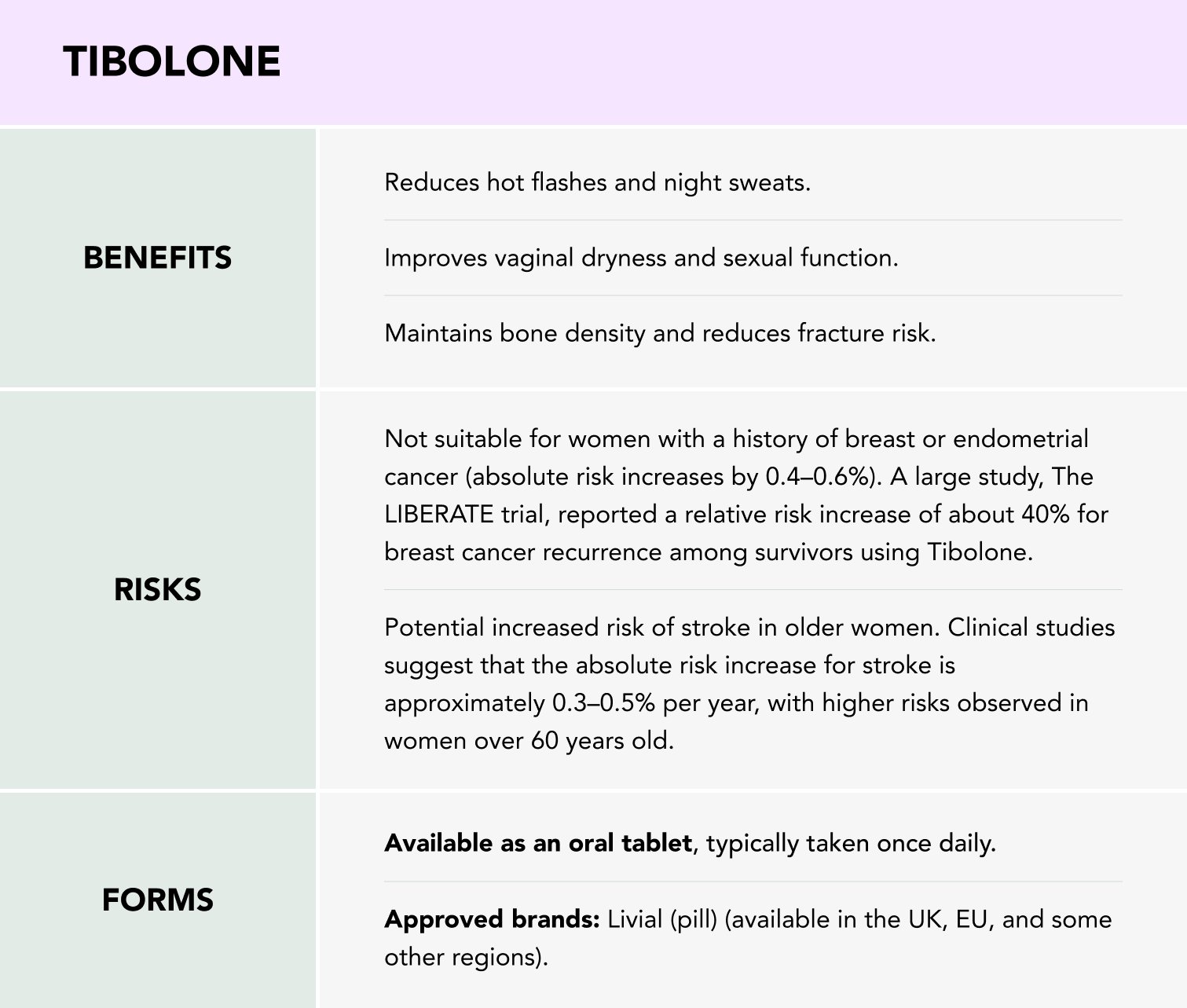
Tibolone was first approved for medical use in Europe in the early 1980s. It was introduced as a treatment for menopausal symptoms and for the prevention of osteoporosis. It quickly gained popularity due to its multi-faceted hormonal effects.
Tibolone is a synthetic steroid with estrogenic, progestogenic, and androgenic properties, making it a one-of-a-kind option for managing menopause symptoms. It’s often prescribed for postmenopausal women who cannot tolerate traditional HRT or prefer a single medication to address multiple symptoms13.
When we think of hormone replacement therapy, testosterone often doesn’t come to mind – yet it plays a fascinating role in women’s health. Although traditionally associated with male biology, testosterone is also essential for women, contributing to energy levels, libido, and overall well-being14.
What makes testosterone therapy intriguing is its potential to address issues like low sexual desire, particularly in postmenopausal women. Clinical studies have shown that testosterone, when carefully dosed, can significantly enhance sexual satisfaction and improve mood and energy.
In women, testosterone is usually prescribed as a gel, cream, or patch at much lower doses than for men. Implants are another option but less commonly used.
While testosterone therapy for women is gaining traction in some countries like the UK and Australia, it remains off-label in others, including the US. This means doctors prescribe it based on clinical discretion rather than official approval by the government.
The debate centers on long-term safety. Potential side effects like acne, excessive hair growth, or voice changes need careful monitoring, but when dosed correctly, these risks are minimal.
As research continues to expand, testosterone may find its place as a legitimate and effective option for select menopausal symptoms. It’s a compelling example of how nuanced and individualized hormone therapy can be, reminding us that hormones are never just one-size-fits-all.
When it comes to HRT, the sheer variety of options can be both empowering and intimidating. My advice? Start with the basics: know your symptoms, understand your medical history, and work closely with a healthcare provider who truly listens.
No option is perfect, but with the right guidance, HRT can be a powerful tool to reclaim comfort, vitality, and balance during the menopause transition
Dr. Jūra Lašas
1.
Baber, R. et al. 2016 IMS Recommendations on women’s midlife health and menopause hormone therapy. (2016) https://doi.org/10.3109/13697137.2015.1129166
2.
Faubion, S. et al. The 2022 hormone therapy position statement of The North American Menopause Society. (2022) https://doi.org/10.1097/GME.0000000000002028
3.
Marjoribanks, J. Long-term hormone therapy for perimenopausal and postmenopausal women. (2017) https://doi.org/10.1002%2F14651858.CD004143.pub5
4.
Hamoda, H. British Menopause Society tools for clinicians: Progestogens and endometrial protection. (2022) https://doi.org/10.1177/20533691211058030
5.
Ross, R. et al. Effect of Hormone Replacement Therapy on Breast Cancer Risk: Estrogen Versus Estrogen Plus Progestin. (2000) https://doi.org/10.1097/00006254-200007000-00022
6.
Paganini-Hill, A. et al. Endometrial cancer and patterns of use of oestrogen replacement therapy: a cohort study. (1989) https://doi.org/10.1038/bjc.1989.91
7.
Rovinski, D. et al. Risk of venous thromboembolism events in postmenopausal women using oral versus non-oral hormone therapy: A systematic review and meta-analysis. (2018) https://doi.org/10.1016/j.thromres.2018.06.014
8.
Vinogradova, Y. et al. Use of hormone replacement therapy and risk of breast cancer: nested case-control studies using the QResearch and CPRD databases. (2020) https://doi.org/10.1136/bmj.m3873
9.
Rovinski, D. et al. Risk of venous thromboembolism events in postmenopausal women using oral versus non-oral hormone therapy: A systematic review and meta-analysis. (2018) https://doi.org/10.1016/j.thromres.2018.06.014
10.
Panay, N. BMS – Consensus statement: Bioidentical HRT. (2019) https://doi.org/10.1177/2053369119841844
11.
Crandall, C. et al. Safety of vaginal estrogens: a systematic review. (2020) https://doi.org/10.1097/GME.0000000000001468
12.
Pickar, J. et al. Tissue selective estrogen complex (TSEC): a review. (2018) https://doi.org/10.1097/GME.0000000000001095
13.
Modelska, K. et al. Tibolone for postmenopausal women: systematic review of randomized trials. (2002) https://doi.org/10.1210/JCEM.87.1.8141
14.
Renke, G. et al. Cardiovascular Safety and Benefits of Testosterone Implant Therapy in Postmenopausal Women: Where Are We? (2023) https://doi.org/10.3390/ph16040619