How to Manage Hot Flashes and Night Sweats Effectively
Reading time 9 min

Reading time 9 min

Physical symptoms can range from mildly inconvenient to significantly disruptive1. Studies show that 60-86% of women experience symptoms so bothersome that they seek medical care2, 3. The good news? Effective strategies backed by science can help manage the symptoms.
To manage hot flashes and night sweats effectively, consider hormone therapy, FDA-approved non-hormonal medications, lifestyle changes, and stress-reduction techniques like mindfulness and cooling strategies.
Let’s dive into practical ways to address the physical changes you’re experiencing. You should discuss all the risks and benefits of the various tools presented below with your healthcare provider. I cover most significant symptoms and management tools in detail in separate articles under Healthy Body & Mind and Exercise & Nutrition.
Vasomotor Symptoms (VMS) are the most common and recognizable signs of menopause transition. They are called vasomotor symptoms because they involve blood vessels reacting and widening. VMS are directly linked to the hormonal changes your body is going through, especially the drop in estrogen. This drop affects the hypothalamus, the part of your brain responsible for regulating body temperature.
When estrogen levels fluctuate and inevitably drop, the hypothalamus gets “confused”, often overreacting to minor temperature changes and making you feel overheated out of nowhere. It’s like your internal thermostat is malfunctioning, which is why you might suddenly break into a sweat, even in the middle of a cool day8, 9, 10, 11.
Hot flashes are experienced (sometimes up to 20 times a day) by up to 80% of women, and they may last up to 12 years, sometimes late into the 70s4, 5, 6, 7. Hot flashes are sudden sensations of intense heat that can spread across the body, especially the chest, neck, and face, often accompanied by sweating and a flushed appearance. It often comes with sweating and a racing heart and can last from 2 to 30 minutes.
Night sweats are what they sound like: episodes of excessive sweating during sleep experienced by at least 13% of women.
When it comes to managing hot flashes and night sweats, there’s no single solution that fits everyone. What works best often depends on the severity of your symptoms, your personal health history, and your comfort level with different treatments.
Fortunately, a wide range of effective strategies exists – from medical therapies to lifestyle adjustments and mind-body practices. Let’s explore the proven options so you can build a personalized plan that works for you.
Estrogen-based hormone therapies are one of the most effective treatments for VMS12, 13. Such therapies can reduce symptoms on average by more than 75%14. They are generally safe for women under 60 or within 10 years of starting menopause, as long as there are no medical reasons to avoid them.
Only two non-hormone treatments for VMS are FDA approved: Paroxetine mesylate (brand name Brisdelle) and Fezolinetant (brand name Veozah/Veoza)13. Doctors may also prescribe Venlafaxine (Brand name Effexor), Escitalopram (Brand names Lexapro and Cipralex), both antidepressants, or Gabapentin (Brand name Neurontin), an anticonvulsant.
There are only a few direct comparisons between HRT and non-hormone options for VMS relief. In those trials, both HRT and medications like venlafaxine or escitalopram showed similar reductions in hot flash frequency. However, these studies used low-dose oral estradiol (0.5 mg daily) without increasing the dose and may have underestimated HRT’s full potential to reduce hot flashes.
Some practical things to think about, suggested by other women:
Studies show both active smoking and secondhand smoke are tied to a higher chance of VMS. The risk climbs even higher for smokers who are also managing obesity. But quitting smoking before 40 can significantly cut this risk15.
Research suggests that eating a nutritious diet, keeping blood sugar levels steady, and staying active can help lower the risk of bothersome hot flashes and night sweats. Even small, healthy changes in these areas can make a difference16, 17.
Mindfulness and meditation show promise for easing VMS and improving the quality of life during menopause. Many studies support their benefits, though results aren’t completely consistent, so more research is needed to confirm these findings. Overall, mindfulness and meditation offer a potential non-medication option for managing symptoms18, 19.
Research suggests that while herbal supplements like phytoestrogens and black cohosh are popular alternatives to hormone therapy, strong evidence for their effectiveness in reducing VMS is lacking. Overall, there’s no solid proof to recommend herbal supplements as a reliable treatment for VMS20, 21.
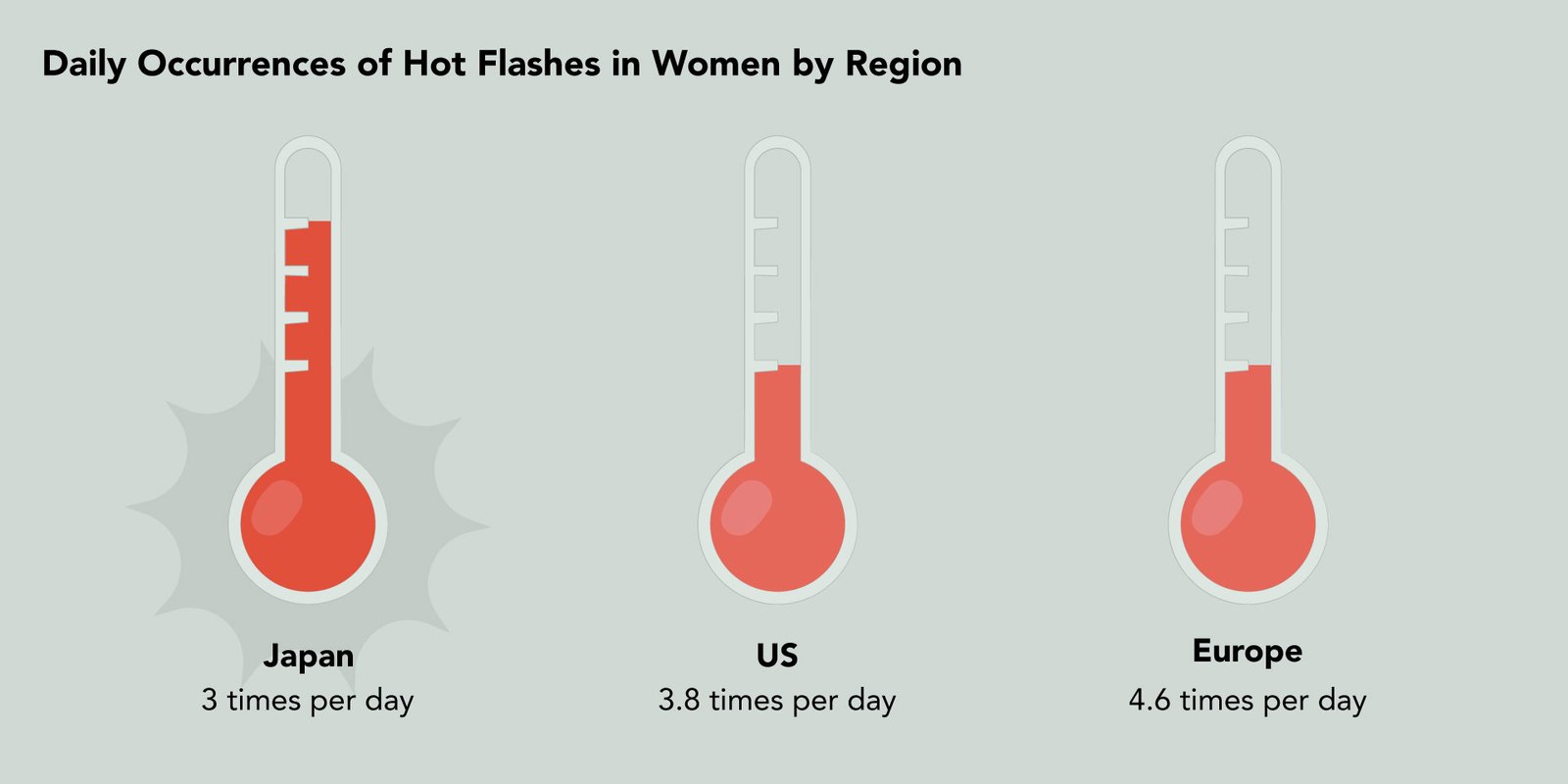
While only 16% of Japanese women experience moderate-to-severe hot flashes and night sweats during menopause much lower than the 34% in the US and 40% in Europe – those Japanese women who do have these symptoms often find them more intense. In fact, 87% of these Japanese women describe their symptoms as severe, compared to most women in Europe and the US who report theirs as moderate.
Additionally, Japanese women have these symptoms less frequently, averaging 3 times per day, whereas women in Europe experience them 4.6 times per day and women in the US 3.8 times per day. This means that although hot flashes and night sweats are less common among Japanese women, the ones who do experience them may have stronger but less frequent episodes22.
Let’s face it – hot flashes and night sweats can feel like your body has betrayed you, but they’re really just your hypothalamus overreacting to hormonal changes. It’s like your internal thermostat is throwing a tantrum. Annoying? Yes. Unmanageable? No.
The good news? You have options. HRT is the gold standard, cutting hot flashes by over 75%, but if hormones aren’t for you, non-hormonal meds like paroxetine, fezolinetant, or even antidepressants like venlafaxine can help.
Not into medication? Small tweaks – like dressing in layers, using cooling pillows, or practicing mindfulness – can make symptoms more bearable. As for herbal supplements like phytoestrogens and black cohosh, the evidence is hit or miss, so they might work for some, but don’t rely on them as a cure-all. It’s all about finding what works best for you.
Finally, I want to emphasize this: menopause is not a one-size-fits-all experience. Cultural differences, lifestyle, and genetics all play a role in how we experience symptoms. What works for someone else might not work for you – and that’s okay. My advice? Start with small, informed steps, talk to your doctor, and find what works best for your unique body and life.
Dr. Jūra Lašas
1.
Laine, C. et al. Menopause. (2009) https://doi.org/10.7326/0003-4819-150-7-200904070-01004
2.
Constantine, G. et al. Behaviours and attitudes influencing treatment decisions for menopausal symptoms in five European countries. (2016) https://doi.org/10.1177/2053369116632439
3.
Williams, R. et al. Healthcare seeking and treatment for menopausal symptoms in the United States. (2007) https://doi.org/10.1016/j.maturitas.2007.09.006
4.
Laine, C. et al. Menopause. (2009) https://doi.org/10.7326/0003-4819-150-7-200904070-01004
5.
Brunner, R. et al. Menopausal symptom experience before and after stopping estrogen therapy in the Women’s Health Initiative randomized, placebo-controlled trial. (2010) https://doi.org/10.1097/gme.0b013e3181d76953
6.
Thurston, R. et al. Vasomotor Symptoms and Menopause: Findings from the Study of Women’s Health across the Nation. (2011) https://doi.org/10.1016/j.ogc.2011.05.006
7.
Soules, M. et al. Executive summary: stages of reproductive aging workshop (STRAW). (2001) https://doi.org/10.1016/S0015-0282(01)02909-0
8.
Politi, M. et al. Revisiting the Duration of Vasomotor Symptoms of Menopause: A Meta-Analysis. (2008) https://doi.org/10.1007/s11606-008-0655-4
9.
Geraghty, P. Vasomotor Symptoms. (2004) https://doi.org/10.1097/01.AOG.0000138795.50777.af
10.
Rapkin, A. Vasomotor symptoms in menopause: physiologic condition and central nervous system approaches to treatment. (2006) https://doi.org/10.1016/J.AJOG.2006.05.056
11.
Gold, E. et al. Longitudinal Analysis of the Association Between Vasomotor Symptoms and Race/Ethnicity Across the Menopausal Transition: Study of Women’s Health Across the Nation American Journal of Public Health. (2006) https://doi.org/10.2105/AJPH.2005.066936
12.
Freedman, M. Quality of life and menopause: the role of estrogen. (2002) https://doi.org/10.1089/15409990260363661
13.
Kling, J. et al. Management of the Vasomotor Symptoms of Menopause: Twofers in Your Clinical Toolbox. (2024) https://doi.org/10.1016/j.mayocp.2024.03.028
14.
Faubion, S. et al. The 2022 hormone therapy position statement of The North American Menopause Society. (2022) https://doi.org/10.1097/GME.0000000000002028
15.
Anderson, D. et al. Obesity, smoking, and risk of vasomotor menopausal symptoms: a pooled analysis of eight cohort studies. (2019) https://doi.org/10.1016/j.ajog.2019.10.103
16.
Tijerina, A. et al. Nutritional Risk Factors Associated with Vasomotor Symptoms in Women Aged 40–65 Years. (2022) https://doi.org/10.3390/nu14132587
17.
Thangwaritorn, P. et al. VASOMOTOR SYMPTOMS AND DIET QUALITY. (2023). https://doi.org/10.1093/geroni/igad104.2452
18.
Garcia, M. et al. The effects of mindfulness and relaxation training for insomnia (MRTI) on postmenopausal women: a pilot study. (2018) https://doi.org/10.1097/GME.0000000000001118
19.
Chen, T. et al. Effectiveness of mindfulness-based interventions on quality of life and menopausal symptoms in menopausal women: A meta-analysis. (2021) https://doi.org/10.1016/j.jpsychores.2021.110515
20.
Newton, K. et al. Treatment of Vasomotor Symptoms of Menopause with Black Cohosh, Multibotanicals, Soy, Hormone Therapy, or Placebo. (2006) https://doi.org/10.7326/0003-4819-145-12-200612190-00003
21.
Annals of Internal Medicine. Treating Symptoms of Menopause: A Study of the Effectiveness of Black Cohosh Alone and with Other Herbal Therapies or Soy. (2006) https://doi.org/10.7326/0003-4819-145-12-200612190-00001
22.
Nappi, R. et al. Global cross-sectional survey of women with vasomotor symptoms associated with menopause: prevalence and quality of life burden. (2021) https://doi.org/10.1097/GME.0000000000001793