Menopause Research: Finally Getting the Scientific Attention It Deserves
Reading time 11 min.
Reading time 11 min.
For decades, menopause research sat in the scientific shadows: understudied and often dismissed. The past decade has witnessed an explosion in menopause research that’s reshaping how we understand and manage this universal transition. From hormone therapy comebacks to breakthrough non-hormonal treatments, science is finally giving menopause the attention it deserves and the findings are empowering.
What is menopause research showing today?
Researchers are uncovering new insights into hormone therapy, non-hormonal treatments, brain changes, and heart health during menopause. These findings are reshaping care and giving women more tools to manage symptoms and long-term health.
While media headlines often spotlight the symptoms we know all too well: hot flashes, brain fog, vaginal dryness; the real action is happening deep in labs and scientific journals. Researchers are digging into the biology of menopause transition with new urgency.
They’re asking bolder questions: Can we target FSH to protect our bones? Can brain imaging help predict who’s at risk of Alzheimer’s? Could we one day delay or even reverse the effects of ovarian aging?
Let’s start with the most misunderstood topic: hormone replacement therapy (HRT) or menopausal hormone therapy (MHT) as a rebranded term.
For years, hormone therapy was feared. After the early 2000s Women’s Health Initiative (WHI) study raised red flags about breast cancer and heart disease, HRT use plummeted. But fast-forward two decades, and the picture looks very different1.
Recent re-analyses of the original WHI data and dozens of new studies now confirm that for most healthy women under 60 or within 10 years of menopause, HRT is not only safe, but beneficial. It’s the most effective treatment for vasomotor symptoms (hot flashes, night sweats), helps prevent bone loss, and may even support heart and brain health when started at the right time.
Key updates:
Even the North American Menopause Society now states that HRT is a valid option, especially for women struggling with symptoms or at risk of osteoporosis2. And the fear-based messaging? It’s being replaced by individualized care, informed by science not stigma.
Not every woman can or wants to take hormones. Until recently, non-hormonal options felt limited, underwhelming, and mostly off-label. This has changed.
In 2023, the FDA approved fezolinetant, the first non-hormonal drug specifically designed to treat hot flashes. It targets the neurokinin B pathway in the brain: the one responsible for your internal thermostat suddenly going haywire. In large clinical trials, women taking fezolinetant had up to 60% fewer hot flashes in just 4 weeks. Side effects were mild, and it doesn’t affect breast or uterine tissue3.

Other non-hormonal therapies now gaining traction:
For women who’ve been told, “just deal with it” this new science says otherwise.
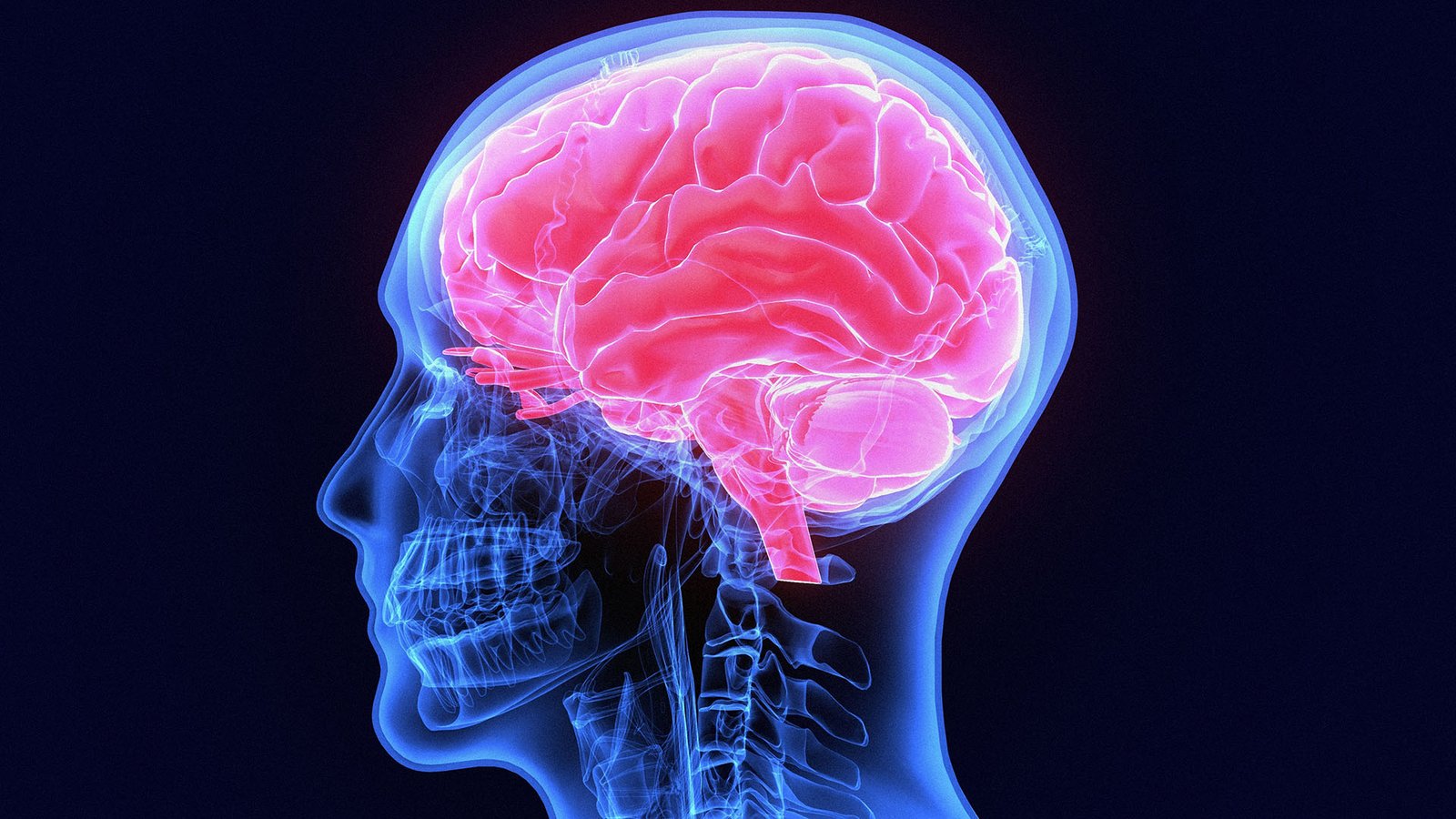
Many women describe brain fog as frustrating, embarrassing, and sometimes scary. Trouble concentrating. Lost words. Slower thinking. These symptoms aren’t a lack of organization. It’s biology, baby!
“Recent neuroimaging studies show that menopause changes the structure and activity of the brain.“
Estrogen withdrawal affects regions responsible for memory, thermoregulation, and cognition. Perimenopause is associated with a decrease in brain volume and energy use. However, these changes are not permanent, the brain adapts post-menopause4,5.
A landmark 2024 analysis of over 230,000 women found that those who experienced menopause before age 40 had a 47% higher risk of developing dementia later in life6. The pattern was clear: the younger the menopause, the higher the dementia risk. This elevated risk was comparable to well-established risk factors like smoking or having a stroke.
Good news: scientists found that women who start HRT in midlife showed a 32% lower risk of later dementia, while those who started it after age 65 showed increased risk7. Estrogen can protect the brain but only if introduced when neural aging is just beginning.
Cardiovascular disease is the leading cause of death in women, and menopause accelerates the risk. Menopause transition changes everything: your heart, cholesterol, body fat, and insulin sensitivity too. And it starts before your periods fully stop8.
During the menopause transition, researchers have documented a sharp rise in LDL (“bad”) cholesterol, abdominal fat, and insulin resistance. These changes are linked directly to hormonal shifts, not just aging. As estrogen declines and FSH rises, many women experience weight gain around the middle, worsening cholesterol and blood sugar levels9. Hot flashes aren’t just a nuisance either. Frequent flashes have been linked to a higher risk of heart disease and stroke later in life.
What can help?
Menopause doesn’t doom you to heart disease or diabetes but ignoring its effects might.
Science is catching up to what women have known all along: menopause affects every part of you. It’s not “just hot flashes.” It’s your brain, your heart, your bones, your mood, your sleep, your identity. What excites me most is the shift in perspective. Menopause is no longer viewed as just a collection of annoying symptoms to endure, but as a critical window that influences decades of health to come. This knowledge is power! It means we can be proactive rather than reactive.
We have treatments that work, both hormonal and non-hormonal. We have emerging therapies that target the brain, metabolic pathways, even aging itself. What we need next is for every woman to have access to this information and to a healthcare system that takes her concerns seriously.
That’s why I created this platform. So you can understand what’s happening in your body, and make decisions based on facts not fear.
Dr. Jūra Lašas
1.
Manson, J. et al. Menopausal Hormone Therapy and Health Outcomes During the Intervention and Extended Poststopping Phases of the Women’s Health Initiative Randomized Trials. (2017) https://doi.org/10.1001/jama.2017.11217
2.
Faubion, S. et al. The 2022 hormone therapy position statement of The North American Menopause Society. (2022) https://doi.org/10.1097/GME.0000000000002028
3.
Lederman, S. et al. Fezolinetant for treatment of moderate-to-severe vasomotor symptoms associated with menopause (SKYLIGHT 1). (2023) https://doi.org/10.1016/S0140-6736(23)00085-5
4.
Zhang, S. et al. Subcortical Volume Changes in Early Menopausal Women and Correlation With Neuropsychological Tests. (2021) https://pubmed.ncbi.nlm.nih.gov/34955807/
5.
Mosconi, L. et al. Menopause impacts human brain structure, connectivity, energy metabolism, and amyloid-beta deposition. (2021) https://doi.org/10.1038/s41598-021-90084-y
6.
Dobson, A. et al. Age at menopause and risk of dementia. (2024) https://doi.org/10.1093/ageing/afae254
7.
Marjoribanks, J. et al. Long-term hormone therapy for perimenopausal and postmenopausal women. (2017) https://doi.org/10.1002/14651858.cd004143.pub5
8.
Marlatt, K. et al. Body composition and cardiometabolic health across the menopause transition. (2022) https://doi.org/10.1002/oby.23289
9.
El Khoudary, S. et al. Increase in visceral adiposity during the menopausal transition. (2015) https://doi.org/10.1210/jc.2015-2110
10.
Taylor, S. et al. Is it time to revisit the recommendations for initiation of menopausal hormone therapy? (2025) https://doi.org/10.1016/s2213-8587(24)00270-5