Science Basics for Menopause Health: Simply Explained
Reading time 11 min

Reading time 11 min

Science. It’s a word that gets thrown around a lot, but what does it really mean? Understanding science basics for menopause health can help you navigate symptoms, treatments, and advice with real confidence. Let’s break it down together.
Why do science basics matter for menopause health?
Understanding science basics helps you filter health advice, trust clinical research, and make better menopause-related decisions based on evidence, not just trends.
At its core, science is just a way to figure things out – reliably and systematically. Imagine you’re trying to figure out which moisturizer works best for your skin. You wouldn’t just pick one randomly and declare it the best, right? You’d try a few, see how your skin reacts, and then decide. That’s science in action!
Scientists observe the world, ask questions, test ideas, and then (here’s the key part) look at the evidence before drawing conclusions. It’s not about gut feelings or trends. It’s about facts and proof1.
You might be wondering, “Okay, but how does this apply to my body changing with menopause?” The answer: in every way possible. Menopause research is built on decades of science.
Understanding the basics of how science works can help you navigate this stage of life with confidence. Instead of being overwhelmed by conflicting information, you’ll be able to sift through the noise and focus on what’s truly backed by evidence.
When it comes to health, not all studies are created equal. You’ve probably heard of clinical trials. These are considered the best, especially a specific type called a Randomized Controlled Trial (RCT). In an RCT, scientists take a group of people, randomly assign some to receive treatment and others to a placebo (a “dummy” treatment), and then compare the results2.
Double-blind means neither the participants nor the scientists know who’s getting the real treatment and who’s getting the placebo. This helps avoid bias. The bottom line? RCTs are reliable. If a menopause treatment passes one of these trials, it’s worth paying attention to.
Not all studies are created equal, and science has its own hierarchy of evidence3. Picture it as a pyramid:
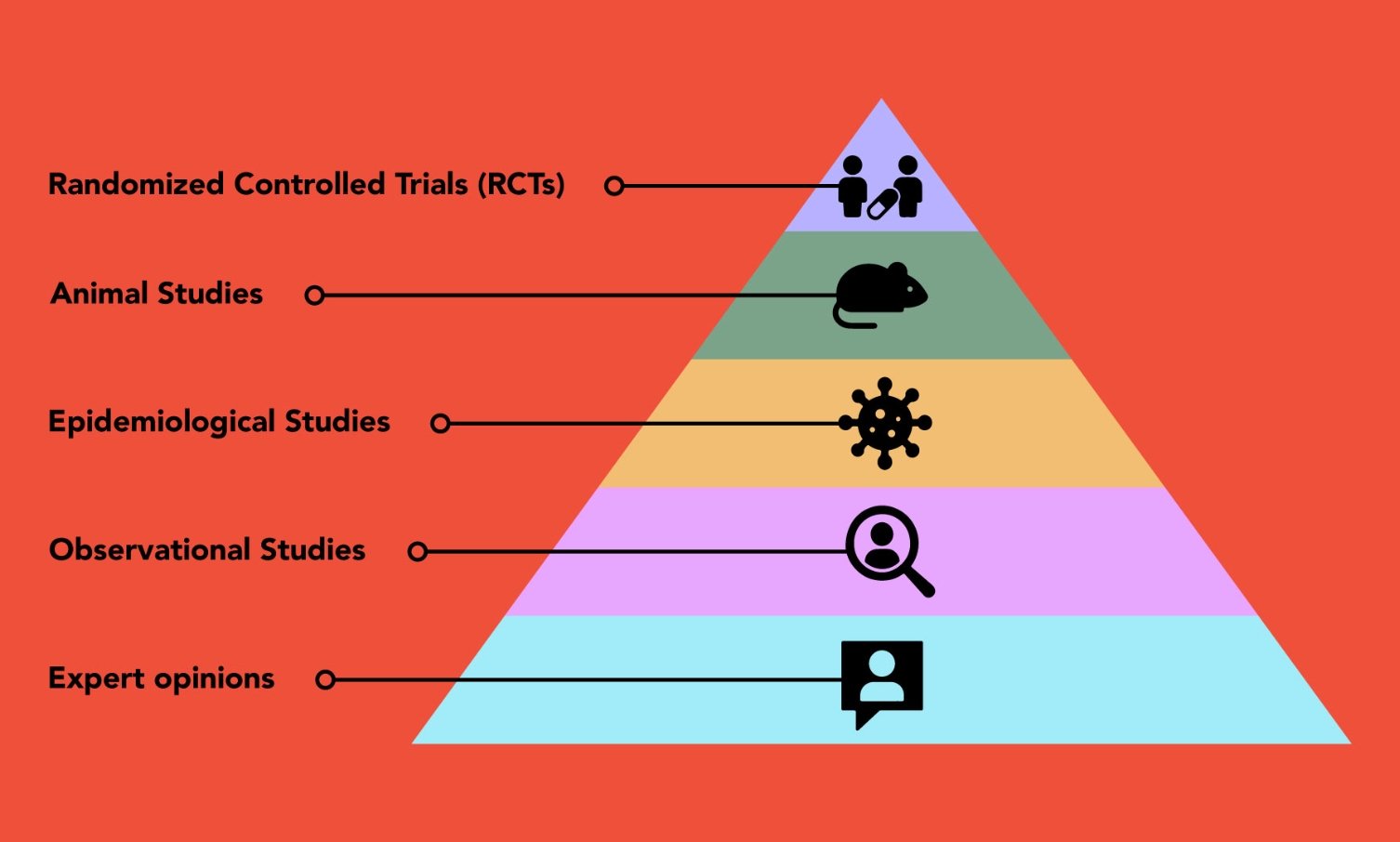
At the bottom, you have expert opinions and anecdotes, personal stories, or professional experiences. They can be interesting, but they don’t hold much weight when it comes to proving anything scientifically.
A bit higher up, we have observational studies. These studies are useful for spotting trends and correlations, but they can’t prove that one thing directly causes another. For example, observational research might show that women who exercise tend to feel better during menopause, but it doesn’t prove that exercise alone is responsible.
Epidemiological studies fall into the same level as observational studies. These studies look at large populations to identify risk factors and health outcomes. They help to establish broad patterns like the age of onset for menopause or associations between lifestyle factors and menopause symptoms. While valuable, these studies also don’t prove direct cause and effect. However, they can guide future research.
Animal studies come next. These involve testing treatments or hypotheses in animals to get a sense of how something might work in humans. Although animals aren’t a perfect match for humans, these studies are crucial for understanding biological mechanisms. For example, much of what we know about hormone therapy came from early animal research.
Above that are Randomized Controlled Trials (RCTs) – the gold standard for scientific evidence. These studies carefully compare treatments to placebos, reducing bias and making their findings more trustworthy.
“A separate bucket that draws data from different research, would be systematic reviews and metanalyses. These are like the superheroes of scientific research. A systematic review pulls together all the studies on a particular topic, evaluating their quality and summarizing the findings”4
A metanalysis goes even further: it combines the data from multiple studies into one big analysis to get a clearer, more powerful result. This means that if a treatment has passed a metanalysis, it’s not just good, it’s been tested and verified by pooling together a lot of high-quality evidence5.
So, when you hear about the latest “miracle cure” for menopause symptoms, ask yourself: Has it been through a randomized trial? Has there been a metanalysis? The more rigorous the research, the more you can trust it.
Let’s say you see a post on social media where someone claims that a particular herbal supplement completely “cured” their hot flashes overnight. This is a personal anecdote, and while it might sound compelling, it’s just one person’s experience. It doesn’t mean the supplement works for everyone, or even that it truly worked for them (it could be a coincidence or a placebo effect).
Compare that to a randomized controlled trial (RCT) where scientists give one group of women the supplement and another group a placebo, tracking their symptoms over several months. If the supplement consistently reduces hot flashes in the group receiving it (and not just the placebo group), that’s a strong sign it’s effective. Better yet, if several RCTs are reviewed in a meta-analysis, the combined data would give an even stronger conclusion.
The lesson? While social media is full of hearsay and anecdotes, solid scientific evidence comes from well-designed studies, not just one-off personal stories.

Before a study gets published, it’s scrutinized by other experts in the field (peer review). These experts check the study’s methods and results to make sure everything is solid. This process helps weed out poor-quality research and ensures that what you’re reading has been evaluated by professionals.
Now, it’s true, that science hasn’t always gotten everything right on the first try. But here’s the thing: it’s the best tool we have for uncovering the truth. Science is designed to correct itself over time.
Yes, conclusions may shift as more research comes out, but that’s exactly how we get closer to the truth. With time and more studies, the evidence becomes stronger, and the real answers emerge. Science may not be perfect, but it’s constantly improving and that’s why it’s worth trusting6.
Science is never “finished.” What we know today might evolve as new research emerges. That’s why you might hear conflicting information. First one study says something is bad for you, and then a few years later, another says it’s okay. This isn’t because science is unreliable; it’s because we’re constantly learning and improving.
A perfect example is the Women’s Health Initiative (WHI) study on hormone replacement therapy (HRT)7, 8. Back in the early 2000s, the WHI study made headlines when it suggested that HRT increased the risk of breast cancer, heart disease, and strokes.
Understandably, many women and healthcare providers were alarmed, and HRT use dropped significantly. However, the study’s findings were later re-examined, and further research showed that the original results had some limitations.
For instance, the study primarily involved older women who had started HRT long after menopause. Newer research has shown that for women who begin HRT earlier (within 10 years of menopause), the risks are lower and the benefits can outweigh those risks.
HRT is particularly beneficial for relieving menopausal symptoms. Metanalyses combining multiple studies have since provided a clearer picture, showing that when used appropriately, HRT can be safe and beneficial for many women.
So, while science didn’t get it exactly right the first time, the truth emerged with more time and research. Science may not be perfect, but it evolves and refines itself, which is exactly how we get closer to the most reliable answers.
Science helps you make decisions based on facts, not guesses or trends. Understanding the basics, like why randomized controlled trials and metanalyses matter, empowers you to make more informed health decisions. And when you’re dealing with the complexities of perimenopause and postmenopause, you deserve the best, most reliable information.
So the next time you hear about a new study on menopause, ask yourself: What’s the evidence? Was it tested in a rigorous clinical trial? Is this based on a systematic review or metanalysis? When you approach your health like a scientist, you’re in the driver’s seat, navigating this journey with confidence.
Dr. Jūra Lašas
1.
Harris, E. Science and Science Teaching. (1942) https://doi.org/10.1038/149734A0
2.
Hariton, E. et al. Randomised controlled trials – the gold standard for effectiveness research. (2018) https://doi.org/10.1111/1471-0528.15199
3.
Brighton, B. et al. Hierarchy of Evidence: From Case Reports to Randomized Controlled Trials. (2003) https://doi.org/10.1097/01.blo.0000079323.41006.12
4.
Siddaway, A. et al. How to Do a Systematic Review: A Best Practice Guide for Conducting and Reporting Narrative Reviews, Meta-Analyses, and Meta-Syntheses. (2019) https://doi.org/10.1146/annurev-psych-010418-102803
5.
Barker, F. et al. Synthesizing medical evidence: systematic reviews and metaanalyses. (2005) https://doi.org/10.3171/FOC.2005.19.4.6
6.
Rosman, T. et al. Belief updating when confronted with scientific evidence: Examining the role of trust in science. (2023) https://doi.org/10.1177/09636625231203538
7.
Neves-e-Castro, M. et al. Results from WHI and HERS II – Implications for women and the prescriber of HRT. (2002) https://doi.org/10.1016/s0378-5122(02)00214-1
8.
Manson, J. et al. Menopausal Hormone Therapy and Health Outcomes During the Intervention and Extended Poststopping Phases of the Women’s Health Initiative Randomized Trials. (2013) https://doi.org/10.1001/jama.2013.278040